![]() STATE OF NEW YORK
STATE OF NEW YORK
DEPARTMENT
OF HEALTH
eMedNY
Prospective
Drug Utilization Review/
Electronic
Claims Capture and Adjudication
ProDUR/ECCA
Provider Manual
![]() STATE OF NEW YORK
STATE OF NEW YORK
DEPARTMENT
OF HEALTH
eMedNY
Prospective
Drug Utilization Review/
Electronic
Claims Capture and Adjudication
ProDUR/ECCA
Provider Manual
TABLE OF CONTENTS
Section
2.4 Electronic
Claims Capture and Adjudication (ECCA)
2.5 Medicare
and Third Party Claims
Chart 1 –
Recipient with Coverage Codes H, K, M, O or ALL on file
Chart 2 -
Recipient without Coverage Codes on file
2.6 Rebills/Adjustment
Information
2.8 Health
Care Financing Administration Common Procedure Coding System (HCPCS)
2.10 Dispensing
Validation System
2.11 Prior
Auth Type Code and Prior Auth Number Submitted
2.12 Temporary
Medicaid Authorizations
2.13 Excess
Income/Spenddown Claims
2.14 Duplicate
Claim Transactions
Reason For
Service (Conflict Code)
Other
Pharmacy Indicator (529-FT)
Previous Date
of Fill (530-FU)
Quantity of
Previous Fill (531-FV)
Other
Prescriber Indicator (533-FX)
Conflict Code
Free Text Descriptions
4.2 Utilization
Threshold (UT) Override
5.0 Pro-DUR/ECCA Input Information
6.0 PRO-DUR/ECCA RESPONSE MESSAGES
7.0 PRO-DUR/ECCA REVERSAL/CANCEL
TRANSACTIONS
9.0 MEVS ACCEPTED CODES - TABLE 1
10.0 MEVS DENIAL CODES - TABLE 2
11.0 CO-PAYMENT CODES - TABLE 6
12.0 Rx DENIAL CODES - TABLE 7
13.0 PHARMACY UT/P & C CODES - TABLE
8
14.0 DISPENSING VALIDATION SYSTEM REASON
CODES - TABLE 9
15.0 PEND REASON CODES – TABLE 10
17.0 GLOSSARY OF ABBREVIATIONS AND TERMS
Personal
Identification Number Request
Certification
Statement For Provider Utilizing Electronic Billing
The New York State Department of Health (DOH) has implemented a program that allows the pharmacy community to submit MEVS transactions in an online real-time environment that performs a Prospective Drug Utilization Review (Pro-DUR). This program was implemented on June 1, 1994 and is currently being administered by the eMedNY contractor. In order to receive payment for services rendered, all pharmacies must submit their transactions through the online ProDUR system. An optional feature of the ProDUR program is the Electronic Claim Capture and Adjudication (ECCA) of claims by the eMedNY contractor. The purpose of the Pro-DUR program is to be in compliance with OBRA 90 mandated Pro-DUR requirements. This program will check all prescriptions with prescription drugs the recipient has taken over the past 90 days and alert the pharmacists to possible medical problems associated with dispensing the new drug.
The telecommunication standards for the Pro-DUR/ECCA system are the same as those recommended by the National Council for Prescription Drug Program, Inc. (NCPDP) and named under the Health Insurance Portability and Accountability Act of 1996 (HIPAA). Only the NCPDP 5.1 Telecommunications standard and the 1.1 Batch formats are supported. The New York State format specifications were developed by using the Official Release of the NCPDP Version 5 Release 1 standard and the 1.1 Batch standard. The NCPDP Official Release is available to NCPDP members from the following address:
National Council for Prescription Drug Programs Inc.
9240 East Raintree Drive
Scottsdale, AZ 85260
(480) 477-1000
The mandatory Pro-DUR/ECCA program was implemented June 1, 1994 and is currently being administered by the eMedNY contractor. In order to receive payment for services rendered, all pharmacies must submit their transactions through the online Pro-DUR program using the NCPDP transaction format. Each pharmacy must choose an access method for these transactions. It is also each pharmacy's decision as to whether the transactions go directly to the eMedNY contractor or through a switch company, which in turn sends the transactions to the eMedNY contractor for processing.
Each online claim transaction is processed through the eligibility edits first, then through the Utilization Threshold (UT), Post and Clear (P&C), DUR, and Dispensing Validation System processing, if warranted. An accepted transaction gives you all the necessary UT, P&C and DUR authorizations in addition to recipient eligibility information. There is no need to do an eligibility or UT service authorization inquiry on the Verifone Omni 3750 Terminal or via telephone.
If you are already processing your transactions online, you should not be sending the same transaction through the Verifone Omni 3750 Terminal (transaction 1). This causes two service authorizations to be issued and increases the UT counts for the recipient. A recipient could reach his/her UT limit in error if double service authorizations were posted.
The Pro-DUR/ECCA online system is an adjudication system.
The dollar amount returned in the online response is not the amount that you
will be paid. It is the maximum reimbursable unit price amount.
The online system was designed to allow for capture and adjudication of the electronic submission. It is each pharmacy's option as to whether the claim data should be immediately captured online by the eMedNY contractor for payment or if the actual claim will be sent by the provider using paper, magnetic media or electronically, via Batch Pharmacy Dial-Up.
There are three potential access methods for submission of claims through the DUR system:
· PC to host - your Personal Computer will directly dial the MEVS host.
· CPU to CPU - your computer system has a dedicated communication line directly into the MEVS host processor.
· CPU to CPU through a switching company - your Personal Computer will access the MEVS host through a switching company. This access could be through dial up or leased line. The switching company will have a direct line into the MEVS host processor.
Providers must select one of the alternate access methods. If they choose not to use a switching company, they must become certified with the eMedNY contractor to verify their ability to access and process within the MEVS system. Submission via PC-Host or CPU-CPU access (switch or direct) allows up to a maximum of four claims per transaction.
Note: Switching companies or software vendors may restrict claims per transaction to less than four.
Pharmacies selecting the PC-to-Host access method must call 1-800-343-9000 to request a contract and certification package. If choosing to access through a switch, pharmacies must notify the switch and the switch company must notify the eMedNY contractor of the pharmacy’s name and MMIS provider number.
Once a pharmacy has selected an alternate access method,
they will receive communication protocol information from the eMedNY contractor
or from their switching company. For more information on these access methods
OR if you would like a copy of the Pro-DUR/ECCA Standards Manual please contact
the Provider Services Department at
1-800-343-9000.
The card swipe function will still be available on the Verifone Omni 3750 Terminal for pharmacy providers who are designated by NYSDOH Quality Assurance and Audit Office as card swipe providers. Designated pharmacies must swipe the recipient's card on the Verifone Omni 3750 Terminal using transaction type 5, prior to entering the online DUR transaction. No DATA should be entered on the Verifone Omni 3750 Terminal. The eMedNY contractor will match the transactions to ensure that a swipe was performed. Only transaction type 5 will register and match the swipe to the online DUR transaction. The swipe only has to be done once for each recipient per date of service, regardless of the number of prescriptions being filled that day for that particular recipient.
Responses will be returned via the same alternate access method as the input transaction. The response for each claim will either be accepted or rejected. If the claim is rejected, reject codes will be provided to identify the nature of the problem.
If the claim has passed all edits and is acceptable, a C (Captured) will be returned in the prescription (claim) response status code. Each prescription (claim) in the transaction will have a prescription response. If multiple claims are entered on one transaction, it is possible some will be "C" and some will be "R" (Reject). The presence of a "C" does not mean that the claim has been electronically captured for adjudication by the eMedNY contractor. Refer to the ECCA section, on page 2.4.1 for further information.
Reject codes may appear in one or more of the following fields: NCPDP Reject Codes will be returned in the Reject Code (511-FB) field. MEVS Accepted and Denial Codes listed in Table 1 (page 9.0.1) and Table 2 (page 10.0.1), Rx Denial codes listed in Table 7 (page 12.0.1), UT/PC Codes listed in Table 8 (page 13.0.1), DVS codes listed in Table 9 (page 14.0.1), and the Pend Reason Codes listed in Table 10 (page 15.0.1) will be returned in the Additional Message Info (526-FQ) field. If a claim is rejected, an NCPDP Reject Code will always be returned in the Reject Code (511-FB) field and may have a corresponding MEVS Code placed in the Additional Message Info (526-FQ) field to further clarify the error. Both fields should always be reviewed. The valid NCPDP and MEVS Codes can be found in the tables at the end of this manual.
DUR denials will be returned via the rejected response format and will be found in the DUR/PPS Segment data fields. DUR warnings can be returned in both the approved and rejected response formats. Each submitted claim could have three (3) possible DUR responses. If a claim has three denial responses and also has warnings, only the denials will be returned. Additional information on DUR Response Data can be found in the Pro-DUR Processing section.
Note: 5.1 NCPDP Eligibility transactions do not validate the Prescribing Provider's enrollment in the Medical Assistance Program. In addition, they do not verify the Referring Provider for managed care enrollees and clients that are restricted to certain Providers.
The Electronic Claim Capture and Adjudication feature is optional. Providers may elect to have their online claims captured electronically by the eMedNY contractor for editing and final adjudication.
Captured claims will be fully edited for completeness and validity of the format of the entered data. There is a possibility that claims captured by the eMedNY contractor for final adjudication may be pended and subsequently denied. When a captured claim is pended, final adjudication results will appear on the remittance statement produced from the eMedNY contractor processing cycle in which the claim either approved for payment or denied. All claim processing edits are performed during the adjudication process. An advantage of ECCA is that it saves the pharmacy from having to file the claims separately.
Pharmacies that choose to use the ECCA option must select a Personal Identification Number (PIN) and forward that number to NYSDOH for processing. The PIN selection form can be found in the FORM section at the end of this manual. Additionally, the pharmacy must also have an Electronic Transmitter Identification Number (ETIN) (a/k/a TSN or Transmission Supplier Number) on file with the eMedNY contractor. To obtain an ETIN, or for more information, call (518) 447-9256. Remittances for claims submitted for ECCA will be returned to you via the media you select for that ETIN. If you choose your own ETIN, you can select paper or tape remittance. Once the eMedNY contractor has assigned you an ETIN, you must complete a Certification Statement, have it notarized and returned to the eMedNY contractor. The Certification Statement can be found in the FORM section at the end of this manual.
If you wish your claim electronically captured, you must enter the required data in the Processor Control Number (104-A4) field. The required data is the Read Certification Statement, Pharmacist's Initials, PIN, and ETIN. Further details of all input fields are explained in the input data section of this manual.
If the Processor Control Number (104-A4) field is completed properly and the claim is not rejected for an edit, an invoice number is assigned to the claim. This 9-digit number will be returned in the Authorization Number (503-F3) field of the response. Only one invoice number will be returned for a transaction, which could include up to four claims. The invoice number will appear on your remittance statement. If the Processor Control Number (104-A4) field is completed and an invoice number was not returned in the Authorization Number (503-F3) field, the system will return NO CLAIM TO FA indicating that the claim was captured for Service Authorization but not processed for adjudication by the eMedNY contractor.
If a claim has passed all eligibility, UT, P&C, claim history, DUR and DVS editing, a "C" is returned in the response. The NCPDP definition of "C" is Claim Captured. Some software packages may translate this code into words. The only time a claim has been captured for adjudication is if you see an authorization (invoice) number in your response. Claims that have the Authorization Number (503-F3) field assigned online do not have to be submitted on paper, magnetic media or electronic batch. Please note and retain the authorization number of the claim for your records, as the eMedNY contractor may require it for problem investigation. Only claims that do not have an Authorization Number assigned will have to be submitted by the provider directly to the eMedNY contractor, via paper, magnetic media or electronic Batch Pharmacy Dial-Up.
The following types of claims cannot be submitted to the eMedNY contractor for ECCA:
1. An original claim with a date of service more than ninety days old. However, claims over ninety days old will be processed for eligibility, UT and P&C service authorizations, but they need to be sent to the eMedNY contractor on paper, magnetic media or Batch Pharmacy Dial-Up with the appropriate over ninety day reason indicated. Rebills and reversals are allowed to be submitted ECCA with service dates up to two years old.
2. Durable Medical Equipment (DME) claims. DME includes any claim identified by Specialty Code 307. Please Note: DME does NOT include the product supply codes (1 alpha, 4 numeric) found in the MMIS Pharmacy Provider Manual in sections 4.2 and 4.3. Pharmacy DME Claims must be submitted using 837 Professional ASC X12N.
Third Party
A recipient's other insurance information (if any) is returned to you in the online response via the Additional Message field. If the recipient's other insurance covers drugs, either H, K, M, O or the word ALL will be returned in the Insurance Coverage Code position of the Additional Message Field.
For a third party claim to be successfully captured for ECCA via the variable 5.1 format, the Other Coverage Code (308-C8) field and Other Payer Amount Paid (431-DV) field must be entered. Refer to the ProDUR standards for exact formatting of the COB segment. It is extremely important that you make sure that the value entered in the Other Coverage Code field corresponds to the entry in the Other Payer Amount Paid (431-DV) field. The entry in each field must correlate to the other field and be logically correct for your claim to be accepted.
Note: The Other Payer Amount Paid Field is an optional field and should not be submitted unless the recipient has other drug coverage and you have received reimbursement or been notified that the service is not covered by the other insurance company.
The values for field 308-C8 (Other Coverage Code) are:
0 = Not Specified
1 = No Other Coverage Identified
2 = Other Coverage Exists - Payment Collected
3 = Other Coverage Exists - This Claim Not Covered
4 = Other Coverage Exists - Payment Not Collected
5 = Managed Care Plan – Denial
6 = Other Coverage Denied – Not Participating Provider
7 = Other Coverage – Not in Effect at Time of Service
8 = Claim is Billing for Copay
Note: Codes 5
& 6 will be processed as 3.
Code 7 will be processed as 1.
Code 8 will be processed as 2.
There are several edits in place to ensure that logical entries are made in both field 308-C8 and 431-DV. The charts, on the following page, describe what the status of the claim will be based on the field entries. The edits on Chart 1 (page 2.5.2) will occur when the recipient has MEVS Insurance Coverage Codes H, K, M, O or ALL on file with the eMedNY contractor. Chart 2 (page 2.5.3) will occur when no MEVS Insurance Coverage Codes indicating Pharmacy coverage for the recipient are on file.
Medicare
A client’s Medicare information (if any) is returned to you in the online response via the Additional Message field. If Medicare covers the NDC/HCPCS code being dispensed, a claim must be submitted to Medicare first.
For a Medicare Crossover claim to be successfully captured for ECCA via the variable 5.1 format, the appropriate Medicare fields must be entered. Refer to the ProDUR Standards for exact formatting of the COB Segment. The entry in each Medicare field must correlate to the entry in the other Medicare fields and be logically correct for your claim to be accepted.
Note: The Medicare fields are optional fields and should not be submitted unless you have received reimbursement from Medicare.
|
Field 308-C8 Value |
Field 431-DV Value |
NCPDP Format Version |
Field 104-A4 Value |
Claim Status |
|
0,
1, 2, 3, 4, 5, 6, 7, 8 |
431-DV
is Not sent |
51 |
Non-ECCA (Processor Control
Number not sent) or ECCA (Processor Control
Number sent) |
If
all other edits are passed, the transaction will be accepted for issuing
service authorizations and/or DVS prior authorizations. (“C - capture” (field
112-AN) and “NO CLAIM TO FA” (field 503-F3) will be returned). |
|
0,
1, 4 or 7 |
Zeros
or greater |
51 |
ECCA or Non-ECCA |
The
transaction will be rejected. NCPDP
Reject Code: 13 “M/I Other Coverage Code” and Response Code: 717 “Client Has
Other Insurance” will be returned online. |
|
2
or 8 |
Zeros |
51 |
ECCA or Non-ECCA |
The
transaction will be rejected. NCPDP
Reject Code 13 “M/I Other Coverage Code” and Response Code 715 ‘Other Payor
Amount Must Be Greater Than 0’ will be returned. |
|
2
or 8 |
Greater
than Zero |
51 |
ECCA |
If
all other edits are passed, the claim will be approved for payment. (“C -
capture” (field 112-AN) and an invoice number (field 503-F3) will be
returned). Other payor amount will be subtracted from the claim’s payment
amount. |
|
2
or 8 |
Greater
than Zero |
51 |
Non-ECCA |
If
all other edits are passed, the transaction will be accepted for issuing
service authorizations and/or DVS prior authorizations. (“C - capture” (field
112-AN) and “NO CLAIM TO FA” (field 503-F3) will be returned). |
|
3,
5 or 6 |
Zeros,
blank or not sent |
51 |
ECCA |
If
all other edits are passed, the claim will be approved for payment. (“C -
capture” (field 112-AN) and an invoice number (field 503-F3) will be
returned). |
|
3,
5 or 6 |
Zeros |
51 |
Non-ECCA |
If
all other edits are passed, the transaction will be accepted for issuing
service authorizations and/or DVS prior authorizations. (“C - capture” (field
112-AN) and “NO CLAIM TO FA” (field 503-F3) will be returned). |
|
3,
5 or 6 |
Greater
than Zero |
51 |
ECCA or Non-ECCA |
The
transaction will be rejected. NCPDP
Reject Code “13 M/I Other Coverage Code” and Response Code “716 ‘ Other Payor
Amount Must Be Equal to 0” will be returned. |
|
Field 308-C8 Value |
Field 431-DV Value |
NCPDP Format Version |
Field 104-A4 Value |
Claim Status |
|
0,
1, 2, 3, 5, 6, 7 or 8 |
Not
sent |
51 |
Non-ECCA |
If
all other edits are passed, the transaction will be accepted for issuing
service authorizations and/or DVS prior authorizations. (“C - capture” (field
112-AN) and “NO CLAIM TO FA” (field 503-F3) will be returned). |
|
0,
1 or 7 |
Not
sent |
51 |
ECCA |
If
all other edits are passed, the claim will be approved for payment. (“C - capture”
(field 112-AN) and an invoice number (field 503-F3) will be returned). |
|
0,
1, 3, 5, 6 or 7 |
Zeros |
51 |
Non-ECCA |
If
all other edits are passed, the transaction will be accepted for issuing
service authorizations and/or DVS prior authorizations. (“C - capture” (field
112-AN) and “NO CLAIM TO FA” (field 503-F3) will be returned). |
|
0,
1, 7 |
Zeros |
51 |
ECCA |
If
all other edits are passed, the claim will be approved for payment. (“C -
capture” (field 112-AN) and an invoice number (field 503-F3) will be returned). |
|
3,
5 or 6 |
Zeros,
blank or not sent |
51 |
ECCA |
If
all other edits are passed, the claim will be approved for payment. (“C -
capture” (field 112-AN) and an invoice number (field 503-F3) will be
returned). |
|
0,
1, 3, 4, 5, 6 or 7 |
Greater
than Zero |
51 |
Non-ECCA or ECCA |
The
transaction will be rejected. NCPDP
Reject Code “DV - M/I Other Payor
Amount Paid”
and Response Code “320 – Other Insurance Information Inconsistent” will be
returned. |
|
2,
3, 5, 6, or 8 |
Not
sent |
51 |
Non-ECCA or ECCA |
If
all other edits are passed, the transaction will be accepted for issuing
service authorizations and/or DVS prior authorizations. (“C - capture” (field
112-AN) and “NO CLAIM TO FA” (field 503-F3) will be returned). |
|
4 |
Not
sent or zeros |
51 |
Non-ECCA or ECCA |
If
all other edits are passed, the transaction will be accepted for issuing
service authorizations and/or DVS prior authorizations. (“C - capture” (field
112-AN) and “NO CLAIM TO FA” (field 503-F3) will be returned). |
|
2
or 8 |
Greater
than Zero |
51 |
Non-ECCA |
If
all other edits are passed, the transaction will be accepted for issuing
service authorizations and/or DVS prior authorizations. (“C - capture” (field
112-AN) and “NO CLAIM TO FA” (field 503-F3) will be returned). |
|
2
or 8 |
Greater
than Zero |
51 |
ECCA |
If
all other edits are passed, the transaction will be accepted for payment. (“C
- capture” (field 112-AN) and an invoice number (field 503-F3) will be
returned). |
|
2
or 8 |
Zeros |
51 |
Non-ECCA or ECCA |
The
claim will reject. NCPDP Reject Code “13 M/I Other Coverage Code” and
Response Code “715 Other Payor Amount Must Be Greater Than 0” will be
returned. |
Rebills will be processed as adjustments to a previously submitted claim that was approved for payment. Rebills cannot be submitted for claims that are pending or were rejected.
NCPDP standards dictate that a rebill must be submitted with a Transaction Code (103-A3) field value B3 and a Transaction Count (109-A9) field of 1 through 4. The number of claim lines contained within the transaction is indicated by the Transaction Count (109-A9) field. (If one claim line is contained in the transaction, the Transaction Count should be 1. If four claim lines are contained in the transaction, the Transaction Count should be 4).
Although you will need to submit all fields required for the original claim transaction, your claims will be matched to the original claim using: Medicaid Provider Identification Number, Cardholder ID, Prescription Number, and Date Filled. If by chance these fields do not define uniqueness, meaning that more than one active claim meeting the criteria resides on the eMedNY contractor’s claims history file, the most recently submitted claim will be selected for adjustment. If you are trying to adjust the older submission, you will need to submit the rebill via paper where you can supply the Claim Reference Number of a specific claim you are trying to adjust.
Rebill transactions can be submitted for service dates up to two years old if the original transaction was submitted directly to the eMedNY contractor. This includes paper, magnetic media and electronic batch as well as online claim submissions.
If the rebill is adjusting a paid claim, the rebill will appear on your remittance statement. If the rebill is adjusting a paid claim, you must complete the Processor Control Number field.
You cannot adjust a non-ECCA claim to become an ECCA claim. The adjustment will apply any updated information, but the adjustment claim will remain a non-ECCA claim and the NO CLAIM TO FA response will be returned to you. If the rebill is adjusting a non-ECCA transaction, the rebill will not appear on your remittance statement.
Rebills will not affect previously established service authorization limits.
Rebills will not be allowed for original claims that generated a DVS prior approval. If a change is needed to a paid DVS claim, then you can submit the adjustment on paper, magnetic media or electronic batch. You may also reverse the original claim and then submit another original transaction with the corrected information.
The New York State Department of Health (NYSDOH) only allows a maximum of five (5) refills on a prescription. All of the refills must be dispensed within 180 days from the date the prescription was written. Claims for refills over 180 days from the date the prescription was written will be rejected.
The New York State DUR Board has established a standard that if a refill is dispensed too early, you will receive a TD WARNING – EARLY REFILL MMDDYY warning in your DUR response. Please note that the TD WARNING – EARLY REFILL MMDDYY response is only a warning, not a DUR denial (reject).
These codes are also referred to as Sickroom Supplies, "Z" codes, or DME item codes and consist of a 5 digit alpha-numeric code. The valid codes can be found in sections 4.2 and 4.3 of the MMIS Pharmacy Provider Manual. For DVS, DME items are only reimbursable under COS 0442. The transaction must be sent through ePACES, Verifone Omni 3750 Terminal or 278 ASC X12N.
The 5 digit alpha-numeric codes must be submitted in the Product/Service Id (407-D7) field along with the Product/Service Id Qualifier (436-E1) field, which identifies the number being sent. A qualifier of ‘09’ must be used in the NCPDP 5.1 format. If the code and the qualifier are not submitted in these fields, your claim will be rejected.
When submitting HCPCS codes, ensure that the following fields are correctly completed:
|
FIELD |
CONTENTS |
|
Compound Code |
Must contain a zero or one. Use zero for DVS transactions. |
|
Product/Service Id Qualifier |
Must contain a value of ’09’. |
|
Product/Service Id |
HCPCS 5 characters in length plus 2 blanks |
A correct entry in the Product/Service Id field would look as follows:
|
Z2500 |
Note: Where bb equal two blanks or BO
modifier.
|
Z2500BO |
When submitting HCPCS if a modifier is required, append to the HCPCS code.
Be aware that the Quantity/Size listed in the MMIS Provider Manual for each HCPCS code is not usually the quantity that should be entered in the Quantity Dispensed (442-E7) field. The quantities listed in the manual refer to ounces, milligrams, sizes, units or the number contained in each unit (box, package, bottles, etc). The entry in the Quantity Dispensed (442-E7) field should be the number of units dispensed.
The following examples are listed to help clarify the correct Quantity Dispensed (442-E7) field entries.
|
HCPCS |
QUANTITY
SIZE IN MANUAL |
QUANTITY
DISPENSED |
MAX QUANTITY |
|
|
Code |
Description |
|||
|
Z2001 |
Butterfly
Clamps |
100's
(up to 1) |
0000001000
(1 box dispensed) |
1
box |
|
Z2003 |
Plastic
Strips |
50's |
0000002000
(2 boxes of 50 dispensed) |
5
boxes |
|
Z2012 |
Adhesive
Tape |
2"
x 5 yd |
0000003000
(3 rolls dispensed) |
5
rolls |
|
A4244 |
Alcohol or peroxide per
pint |
16oz |
0000001000 (1 pint bottle dispensed) |
5
bottles |
|
A4215 |
Needles |
each
(up to 200) |
0000056000 (56 needles dispensed) |
200
needles |
|
A4635 |
Underarm pad crutch
replacement |
each
(up to 2) |
0000001000
(1 pad dispensed) |
2
pads |
Note: Decimals are implied in the Quantity Dispensed field.
The Quantity Dispensed (442-E7) field for enteral products should be entered as caloric units. For example: A prescription is for Regular Ensure 1-8 oz. can/day, 30 cans with five refills. There are 75 caloric units per 30 cans (one month supply). The correct entry for the current date of service is 75000. Do not include refills.
Note: The Quantity Dispensed (442-E7) is a 10 digit field with 7 digits to the left of the decimal and 3 digits to the right.
This function enables suppliers of prescription footwear items, specified drugs, certain medical surgical supplies and durable medical equipment to receive a prior approval number (DVS number) through an automated electronic MEVS system. The DVS transaction can be submitted through the NCPDP 5.1 format. The claims processing system will recognize an item/NDC code requiring a DVS number and will process the transaction through all required editing. If approved, and if the item/NDC code is reimbursable under category of service 0441, 0161 or 0288, the DVS number will be returned in the Additional Message (526-FQ) field and the claim will be processed for adjudication (if ECCA is requested). Only items reimbursable under Category of Service 0441, 0161 or 0288 (Rx) will be processed through ECCA. Items, which are only reimbursable under Category of Service 0442 (DME), cannot be submitted through the NCPDP 5.1 format. The DVS Prior Approval must be requested through the Verifone Omni 3750 Terminal or 278 ASC X12N transaction. The claim must be billed using 837 Professional ASC X12N or paper Claim Form C. Be sure to put the DVS number on the claim.
Important Information Regarding DVS
Transactions
· Transactions for both NDC’s and HCPCS can be submitted using the 5.1 format, if reimbursable under COS 0441, 0161 or 0288.
· Although multiple claim lines per transaction can be submitted, only one DVS claim line item can be submitted per transaction and the DVS line must be the first line item within the transaction.
· Item codes that require a DVS number will not be processed through the UT, P & C or DUR programs. Prescription Drugs that require a DVS number will be subject to UT, P & C and DUR processing.
· Only current dates of service will be accepted for DVS transactions.
The Prior Auth Type Code (461-EU) field is a two (2) position numeric field. There are two values expected by NYSDOH for this field.
01 = Prior Authorization. If this value is used, then Prior Auth Number Submitted (462-EV) field must contain in the first eight positions, a prior approval number followed by zeros to fill the field to eleven.
04 = Exemption from co-pay. Use to indicate the recipient is exempt. If this value is used, the eleven position numeric 462-EV field is submitted unless a previously obtained Prior Approval is being reported on the claim and the recipient is also exempt from co-pay.
The Prior Auth Number Submitted (462-EV) field is an eleven (11) position numeric field. If reporting a prior authorization, use a value (01) in 461-EU field. Send the prior authorization number in the first eight positions and fill the last three
positions with zeros.
If the patient is exempt from co-pay, submit a value (04) in 461-EU field.
Do not send Prior Auth Number Submitted (462-EV) field unless the claim also requires a
prior authorization.
There have been increasing concerns regarding Medicaid provider acceptance of the Temporary Medicaid Authorization (DSS-2831A), especially from pharmacy providers. When an applicant is determined eligible and has an immediate medical need, the local district may issue a Temporary Medicaid Authorization pending the client receipt of a permanent Common Benefit Identification Card.
Please be aware that a mechanism is in place to reimburse providers for rendering services to a client with a Temporary Medicaid Authorization. Providers should first make a copy of all Temporary Medicaid Authorizations for their records. These claims cannot be submitted by pharmacies through the online Pro-DUR/ECCA program because eligibility is not yet on the files and may not have been determined yet. Pharmacy providers must put the letter "M" in the Service Authorization Exception field and submit the claim directly to the eMedNY contractor via paper. The claim will pay upon the local district verifying eligibility in WMS. If the claim pends for client ineligibility, wait for the final adjudication of the claim. This information will appear on your remittance statement. If the final adjudication of the claim results in a denial for client ineligibility, please contact NYS DOH, OMM Local District Support Unit. For Upstate recipients call (518) 474-8216; the number for New York City recipients is (212) 268-6855.
Unlike the Temporary Medicaid Authorizations mentioned on the preceding page, these claims can be submitted through the online Pro-DUR/ECCA program. To properly submit a spenddown claim, the Eligibility Clarification Code (309-C9) field must contain a value of two (2) and the Patient Paid Amount (433-DX) field should contain the amount of the spenddown paid by the recipient, even if that amount is zero. These claims will not be processed through the eligibility edits. If the claim passes all other editing and you have elected the ECCA option, your claim will be captured and pended by the eMedNY contractor waiting for the WMS eligibility file update from the local district to indicate that the spenddown has been met. If the eligibility information does not appear in a timely manner on the eMedNY contractor file, the claim will be denied.
The Eligibility Clarification Code (309-C9) field may also be used to report a Nursing Home Override in those instances where the Client’s file shows residency within an In-State Skilled Nursing Facility that covers pharmacy services. The override procedure may be used to resubmit a previously denied claim. If the Client has been discharged but the eMedNY Contractors’ file shows that the Client still resides in the Skilled Nursing Facility, you may submit an override. This will result in a pend status which will give the local districts time to update the Client’s file. If the update is not received within 30 days, the claim will deny.
When an online claim transaction is sent to the MEVS, it will be matched against previously captured (approved) claims. If the transaction is determined to be an exact duplicate of a previously approved claim, the MEVS will return a “C” in the Transaction Response Status (112-AN) field. The remaining response fields will contain the data that was returned in the original response. The following fields will be examined to determine if the original captured response will be issued:
· Service Provider Number (201-B1 on Transaction Header Segment)
· Cardholder ID Number (302-C2 on Insurance Segment)
· Date of Service (401-D1 on Transaction Header Segment)
· Prescription/Service Reference # (402-D2 on Claim Segment)
· Fill Number (403-D3 on Claim Segment)
· Prior Auth Number Submitted (462-EV on Claim Segment)
· Product/Service ID (407-D7)
If identical data exists only in certain subsets of the above fields, your claim will be rejected for NCPDP Reject Code 83 “Duplicate Paid/Captured Claim” unless prior approval was obtained for one of the two conflicting transactions (meaning Prior Auth Number Submitted (462-EV) field would need to contain a PA Number on one claim, and no PA Number for the other claim.)
For example, a NCPDP Reject Code of 83 “Duplicate Paid/Captured Claim” is returned when a claim is submitted and the Service Provider Number, Cardholder ID, and Prior Approval Number fields match a previous paid claim and one of the following conditions also exists:
· Prescription Service Reference Number matches, but NDC/HCPCS is different.
· NDC/HCPCS matches, but Prescription Service Reference Number is different.
· Prescription Service Reference Number and Fill Number is the same, but the Date of Service is different.
If the original transaction was non-ECCA and the duplicate transaction is ECCA, the transaction response will be the original non-ECCA response. No adjudication process will occur.
A drug history profile is maintained for all recipients. This file contains a record for each accepted prescription or OTC item entered through the ProDUR system. Each prescription on the drug profile is assigned an expiration date. This date is calculated using the date filled plus the days supply.
All prescription and OTC transactions are compared to the recipient's drug profile. If the new prescription falls within the active date range (date filled plus days supply) and a conflict exists, a DUR response will be returned. ProDUR editing is not performed on compound drugs or sickroom supplies. DUR editing will also be performed for the majority of the denial codes on Table 2 (page 10.0.1), Table 7 (page 12.0.1), Table 8 (page 13.0.1) and Table 9 (page 14.0.1).
The DUR edits are based on the clinical database compiled by First DataBank. This information is used to administer the New York State Medicaid Pro-DUR program under the direction of the DUR Board.
Up to three (3) DUR related conflicts can be identified and returned for each drug submitted. Information about these conflicts is returned in the response in order of importance.
Conflicts detected by the Pro-DUR editing may result in reject or warning conditions. At present, there are only two conditions that will cause a requested drug to be rejected: clinical significance (severity) one (1) condition from the Therapeutic Duplication edit and clinical significance one (1) condition from the Drug-Drug Interaction edit. Any other DUR response is a warning and will not cause the claim to be rejected. If a DUR reject is returned for a drug, no DUR, UT, P&C, or DVS authorizations will be retained for the claim. In order to get the necessary authorizations from the Pro-DUR system to dispense a drug that has been rejected by the DUR edits, an override request must be submitted. Overrides are discussed further in the Override Processing section.
The following series of edits are performed by the Pro-DUR system:
Therapeutic
Duplication (TD)
The Therapeutic Duplication edit checks the therapeutic class of the new drug against the classes of the recipient's current, active drugs already dispensed.
Drug-Drug
Interactions (DD)
The Drug-Drug Interaction edit matches the new drug against the recipient's current, active drugs to identify clinically relevant interactions.
Drug-Disease
Contraindications (DC)
The Drug-Disease Contraindications edit determines whether the new drug is potentially harmful to the individual's disease condition. The active drugs on drug history determine the recipient’s disease condition(s).
Drug Pregnancy
Alert (PG)
Drug Pregnancy Alert warnings are returned for females between the ages of 13 and 52 on new drugs that may be harmful to pregnant women.
Pediatric Precautions (PA)
Pediatric Precautions are returned for children under the age of eighteen (18) on new drugs that may be harmful to children.
Lactation Precautions (PG)
Lactation Precautions are returned for females between the ages of 13 and 52 on new drugs that may be harmful to nursing women or their babies.
Geriatric Precautions (PA)
Geriatric Precautions are returned for adults over the age of 60 on new drugs that may be harmful to older adults.
High Dose Alert (HD)
A High Dose Alert is returned if the dosage for the new drug exceeds the maximum dosage recommended for the recipient's age group.
Low Dose Alert (LD)
A Low Dose Alert is returned if the dosage for the new drug is below the minimum dosage recommended for the recipient's age group.
The following information is returned in the response from the Pro-DUR system for each identified DUR conflict:
Drug Conflict Code
(439-E4)
Clinical
Significance (528-FS)
Other Pharmacy
Indicator (529-FT)
Previous Date of
Fill (530-FU)
Quantity of
Previous Fill (531-FV)
Database Indicator
(532-FW)
Other Prescriber
Indicator (533-FX)
Free Text (544-FY)
The Drug Conflict Code identifies the type of DUR conflict found when a new prescription is compared against the recipient's drug history file and demographics. Following are the values that may be returned as Drug Conflict Codes:
TD = Therapeutic Duplication
DD = Drug-Drug Interactions
DC = Inferred Drug Disease Precaution
PG = Drug Pregnancy Alert
PA = Drug Age Precaution
LD = Low Dose Alert
HD = High Dose Alert
The Clinical Significance is a code that identifies the severity level and how critical the conflict. The following chart lists each drug conflict code and the clinical significance codes which may be returned for that code as well as whether they are DUR rejects or warnings.
|
Conflict Code |
Reject/ Warning |
Clinical Significance |
Description of Clinical Significance |
|
TD Therapeutic Duplication |
R |
1 |
An Original Prescription that duplicates a therapy the recipient is already taking. |
|
|
W |
2 |
Prescription is a Refill and is being filled prior to 75% of the prior script's days supply. |
|
DD Drug-Drug |
R |
1 |
Most significant. Documentation substantiates interaction is at least likely to occur in some patients, even though more clinical data may be needed. Action to reduce risk of adverse interaction usually required. |
|
|
W |
2 |
Significant. Documentation substantiates interaction is at least likely to occur in some patients, even though more clinical data may be needed. Assess risk to patient and take action as needed. |
|
|
W |
3 |
Possibly significant. Little clinical data exists. Conservative measures are recommended because the potential for severe adverse consequences is great. |
|
DC Drug Disease |
W |
1 |
Absolute Contraindication. Drug Therapy for the recipient should be changed. |
|
|
W |
2 |
Precaution. The risk/benefit of therapy should be considered and the recipient's response closely monitored. |
|
PG Pregnancy |
W |
D |
PREGNANCY There is positive evidence of human fetal risk based on adverse reaction data from investigation or marketing experience or studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks. |
|
|
W |
X |
PREGNANCY Studies in animals or humans have demonstrated fetal abnormalities and/or there is positive evidence of human fetal risk based on adverse reaction data from investigation or marketing experience, and the risks involved in use of the drug in pregnant women clearly outweigh potential benefits. |
|
|
W |
1 |
PREGNANCY No FDA rating but is contraindicated or not recommended; may have animal and/or human studies or pre- or post-marketing information. |
|
|
W |
1 |
LACTATION Absolute Contraindication. The Drug should not be dispensed. |
|
|
W |
2 |
LACTATION Precaution. Use of the Drug should be evaluated carefully. |
|
PA Drug Age |
W |
1 |
Absolute Contraindication. Drug Therapy should be changed. |
|
LD Low Dose |
W |
1 |
Prescribed dose is less than the minimum appropriate for the drug. |
|
HD High Dose |
W |
1 |
Prescribed dose is greater than the maximum appropriate for the drug. |
The following values may be returned in the Other Pharmacy Indicator:
0 = Not Specified
1 = Your Pharmacy
3 = Other Pharmacy
The Previous Date of Fill provides the date the conflicting drug was dispensed.
The Quantity of Previous Fill provides the quantity of the conflicting drug.
The Database Indicator will always be returned with a value of 1 to indicate that First DataBank is the DUR database provider.
The Other Prescriber Indicator compares the Prescriber of the current prescription to the Prescriber of the conflicting drug from the recipient's active drug profile, and returns one of the following codes:
0 = Not Specified
1 = Same Prescriber
2 = Other Prescriber
A Free Text message is returned for each conflict to provide additional information about the DUR condition. Following is a description of the Free Text:
Note: Bold Text in the examples below represents Free Text.
|
CODE |
FREE TEXT DESCRIPTION |
||||||||||||||||||||||||||||
|
TD |
For Clinical Significance 1, the name, strength, dose form and day’s supply of the conflicting drug from the Drug Profile. |
||||||||||||||||||||||||||||
|
|
Example |
||||||||||||||||||||||||||||
|
|
TD |
1 |
1 |
20020926 |
0000030000 |
1 |
1 |
PROPRANOLOL |
10MG |
TABLET 030 |
|
||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
For Clinical Significance 2 the words WARNING - EARLY REFILL MMDDYY |
||||||||||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
Example |
||||||||||||||||||||||||||||
|
|
TD |
2 |
1 |
20020929 |
0000030000 |
1 |
1 |
WARNING – EARLY REFILL
10/22/02 |
|||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
Note: MMDDYY is the earliest date that the refill should be filled. |
||||||||||||||||||||||||||||
|
DD |
Will contain the Clinical Effect Code followed by the Drug Name from the Drug Profile of the drug interacting with the new prescription being filled. The latter drug will be the new prescription drug and the former drug will be the drug from the Drug Profile. The Clinical Effect Code will consist of one of the following values: Examples of each Clinical Effect code is included. |
||||||||||||||||||||||||||||
|
|
INF Increased effect of former drug |
||||||||||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
Example |
||||||||||||||||||||||||||||
|
|
DD |
2 |
1 |
20021011 |
0000030000 |
1 |
1 |
INF DIGITALIS/KALURETICS |
|||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
DEF Decreased effect of former drug |
||||||||||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
Example |
||||||||||||||||||||||||||||
|
|
DD |
2 |
1 |
20021012 |
0000030000 |
1 |
1 |
DEF |
CORTICOSTEROIDS/BARBITURAT |
||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
INL Increased effect of latter drug |
||||||||||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
Example |
||||||||||||||||||||||||||||
|
|
DD |
3 |
1 |
20021003 |
0000030000 |
1 |
1 |
INL |
VERAPAMIL/DIGOXIN |
||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
DEL Decreased effect of latter drug |
||||||||||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
Example |
||||||||||||||||||||||||||||
|
|
DD |
2 |
1 |
20020920 |
0000060000 |
1 |
1 |
DEL |
NSAID/LOOP DIURETICS |
||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
ARF Adverse reaction of former drug |
||||||||||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
Example |
||||||||||||||||||||||||||||
|
|
DD |
2 |
1 |
20021018 |
0000090000 |
1 |
1 |
ARF |
THEOPHYLLINES/TICLOPIDINE |
||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
ARL Adverse reaction of latter drug |
||||||||||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
Example |
||||||||||||||||||||||||||||
|
|
DD |
1 |
1 |
20021014 |
0000050000 |
1 |
1 |
ARL |
NSAID/TRIAMTERENE |
||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
MAR Adverse reaction of both drugs |
||||||||||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
Example |
||||||||||||||||||||||||||||
|
|
DD |
2 |
1 |
20020920 |
0000090000 |
1 |
1 |
MAR |
ACE INHIBITORS/POTASS.SPAR |
||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
MXF Mixed effects of former drug |
||||||||||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
Example |
||||||||||||||||||||||||||||
|
|
DD |
2 |
1 |
20021018 |
0000015000 |
1 |
1 |
MXF |
ANTICOAGULANTS,ORAL/ANTITH |
||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
MXL Mixed effects of latter drug |
||||||||||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
Example |
||||||||||||||||||||||||||||
|
|
DD |
2 |
1 |
20020919 |
0000060000 |
1 |
1 |
MXL |
HYDANTOINS/DISOPYRAMIDE |
||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
DC |
The description of the drug/disease contraindication. |
||||||||||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
Example |
||||||||||||||||||||||||||||
|
|
DC |
1 |
1 |
20020914 |
0000090000 |
1 |
1 |
HYPERTENSION |
|||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
PG |
For pregnancy precautions the words
PREGNANCY PRECAUTION |
||||||||||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
Example |
||||||||||||||||||||||||||||
|
|
PG |
1 |
0 |
00000000 |
0000000000 |
1 |
0 |
PREGNANCY PRECAUTION |
|||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
For lactation precautions the words
LACTATION PRECAUTION |
||||||||||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
Example |
||||||||||||||||||||||||||||
|
|
PG |
2 |
0 |
00000000 |
0000000000 |
1 |
0 |
LACTATION PRECAUTION |
|||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
PA |
For pediatric precautions the word PEDIATRIC |
||||||||||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
Example |
||||||||||||||||||||||||||||
|
|
PA |
1 |
0 |
00000000 |
0000000000 |
1 |
0 |
PEDIATRIC |
|||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
For geriatric precautions the word GERIATRIC |
||||||||||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
Example |
||||||||||||||||||||||||||||
|
|
PA |
1 |
0 |
00000000 |
0000000000 |
1 |
0 |
GERIATRIC |
|||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
LD |
For low dose precautions the recommended minimum and maximum dosage will be shown. |
||||||||||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
Example |
||||||||||||||||||||||||||||
|
|
LD |
1 |
0 |
00000000 |
0000000000 |
1 |
0 |
3.000 |
12.000 |
||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
HD |
For high dose precautions the recommended minimum and maximum dosage will be shown. |
||||||||||||||||||||||||||||
|
|
|
||||||||||||||||||||||||||||
|
|
Example |
||||||||||||||||||||||||||||
|
|
HD |
1 |
0 |
00000000 |
0000000000 |
1 |
0 |
1.000 |
8.00 |
||||||||||||||||||||
If your claim transaction was rejected due to a DUR conflict and you intend to dispense the drug, you will need to override the conflict (if appropriate). In order to process a DUR override, the same code that was returned as the denial code (Drug Conflict Code) must be placed in the Reason for Service Code (439-E4) field. The DUR Conflict Code being sent as the override must match the DUR Conflict Code received in the response of the original transaction. A corresponding entry must also be entered in the Result of Service Code (441-E6) field. The only conflict codes that are DUR denials and reject the claim are TD (severity level 1) and DD (severity level 1). All of the other codes being returned are warnings and allow your claim to be accepted. Any attempt to override a warning will be rejected. However, we have learned that some software packages are requiring you to do internal overrides for the warnings.
At this time the only rejects that can be overridden are:
TD = Therapeutic Duplication
DD = Drug to Drug Interaction
One of the following values must be used in the Result of Service Code for DUR reject overrides:
1A = Filled as is, false positive
1B = Filled, Prescription as is
1C = Filled with Different Dose
1D = Filled with Different Directions
1E = Filled with Different Drug
1F = Filled with Different Quantity
1G = Filled with Prescriber Approval
DUR Override
Documentation
If a pharmacist overrides a rejected DUR conflict, it is recommended that:
a) The pharmacist writes the date, reason for override and his/her signature or initials on the back of the prescription.
OR
b) If the software permits, comment and electronically store the reason for the override in the patient profile for the specific prescription filled.
If you receive a reject because a recipient is at their
Utilization Threshold service limit (refer to message text field, UT/P&C
codes DA, DD, or DN from Table 8 on page
13.0.1), and you intend to dispense the prescription, you will need to override
the UT limit. To submit a UT override, the provider must resubmit the original
transaction with an entry in the Submission
Clarification Code (420-DK) field. This is the field that replaces the Service Authorization (SA) Exception Code
field currently used for UT overrides when billing the eMedNY contractor on
paper. If multiple claims are submitted in a single transaction, this field
must contain the same value for each claim submitted.
Note: If a UT override is submitted and the recipient has not reached their UT limit, the transaction will be rejected. The following are the only acceptable values to be used in the Submission Clarification Code field if requesting a UT override.
02 = Other Override - use to replace SA Exception code P (Pending an override). If 02 is indicated a "Request for increase in UT Service Limit" must be submitted by the physician or other qualified practitioner.
07 = Medically Necessary - use to replace SA Exception Code J (Immediate Urgent Care) and L (Emergency).
This section describes the input fields required by the New York State Pro-DUR/ECCA system. The way you see this information as you provide input is largely a factor of your computer's software. In fact, some of these field values may be entered on your behalf by your software.
The required header information shown in this section is needed for each transaction request that is sent to the MEVS Pro-DUR/ECCA system.
The NCPDP field numbers are shown in parenthesis at the end of the description for each field.
Following is a description of the fields that must be submitted to the Pro-DUR/ECCA system for each transaction.
|
FIELD |
DESCRIPTION |
|
Bin Number |
All requests must send 004740, which identifies the New York MEVS Pro-DUR/ECCA system.
In most cases, this information is automatically provided by your computer
software. (101-A1) |
|
Cardholder ID Number |
The Cardholder ID Number is the eight position alpha
numeric Medicaid Client Number (CIN) or the thirteen digit Access Number
without the six digit ISO # prefix. Both of these values are provided on the
recipient's benefit card. (302-C2) |
|
Date of Birth |
The Date of Birth is the date the recipient was
born, including the century, which is provided on the recipient's benefit
card. Format = CCYYMMDD (304-C4) |
|
Date of Service |
The Date Filled is the date the prescription was
dispensed. The current date must be used for DVS transactions. (401-D1) |
|
ETIN |
The 3 character Electronic
Transmitter Identification Number entered in the Processor Control Number is assigned to the provider by the
EMedNY contractor. (104-A4) |
|
Patient Gender Code |
The patient gender code
indicates the recipient's gender as follows: 1
= Male 2
= Female (305-C5) |
|
Person Code |
The Person Code is the Sequence
Number found on the recipient's benefit card in the last 2 positions of the
access number. (303-C3) |
|
Pharmacist's Initials |
The Pharmacist's Initials
entered in the Processor Control
Number provides the first
and last initial of the person submitting the claim. (104-A4) |
|
Pharmacy Number |
The Pharmacy Number is an eight
digit Medicaid Provider Identification Number assigned to the pharmacy by the
Department of Health. (201-B1) |
|
PIN |
The four digit PIN entered in
the Processor Control Number is
the Personal Identification Number previously selected by the provider and
submitted to the Department of Health. (104-A4) |
|
Pregnancy Indicator |
This code will specify whether
the patient is pregnant. Valid values are: Blank = Not Specified 1 = Not pregnant 2 = Pregnant (335-2C) |
|
Processor Control Number |
Information entered in the
Processor Control Number is used to indicate that you are requesting Electronic Claim Capture and Adjudication.
The following fields are required by Pro-DUR/ECCA if you are requesting your
claim(s) to be captured for adjudication by the eMedNY contractor. Read
Certification Statement Indicator Pharmacist's
Initials PIN ETIN (104-A4) |
|
Read Certification |
A (Y) entered in the Read
Certification Indicator contained in the Processor
Control Number indicates that you
have read and attest to the agreements in the Certification Statement (refer
to Form Section on page 19.0.1). An "N" indicates that
you have not read the Certification Statement or that you do not agree. (104-A4) |
|
Service Provider Id |
This field must contain the NYS
Medicaid Provider number assigned by NYSDOH (201-B1) |
Service Provider Id Qualifier |
This code will qualify the
entry in the Service Provider Id field (201-B1) as an MMIS Provider ID
number. Acceptable entry is: 05 = Medicaid (Must be submitted in conjunction
with provider number assigned by NYSDOH) (202-B2) |
|
Software Vendor/Certification ID |
Mandatory field used to
identify the software source by switches and/or processors. If not available
or not used between trading partners, then submit 10 spaces. (110-AK) |
|
Transaction Code |
This field identifies the type
of transaction request being submitted. Acceptable codes are: E1
= Eligibility Verification with no claim submitted B1
= Rx Billing P1 = P.A. Request and Billing P4 = Prior Authorization Request Only B2
= Rx Reversal B2 is used to cancel a previous
transaction. Please refer to section on Reversals on page 7.0.1. B3 = Rx
Rebill Note: B3 is used to adjust a
previously paid claim(s). N1 = Rx DUR
only N2 = Rx DUR Reversal N3 = Rx DUR Rebill N1 is used to supply DUR
information only for purposes of updating a recipient's drug history file
when no claim submission or reimbursement is allowed or expected. (103-A3) |
|
Transaction Count |
This field identifies the
number of prescriptions being submitted for a specific transaction. A number
from 1 to a maximum of 4 is allowed dependent on the type of transaction. E1 = Eligibility (1 only) B1 = Billing submit from 1 to 4 B2 = Reversal submit 1 per transaction
for NYS. If reversing a four (4) line
transaction submit each line on a separate B2 transaction. B3 = Rebill submit from 1 to 4. P1 = Billing with P.A. Request submit only
1 P2 = P.A. Reversal submit only 1. P4 = P.A. Request Only submit only 1. N1 = DUR Info Report submit from 1 to 4. N2 = DUR Reversal submit 1 per
transaction. N3 = DUR Rebill submit from 1 to 4. (109-A9) |
|
Version/Release Number |
This identifies the NCPDP
version used for your transaction and is commonly provided by your computer
software. 51 =
Telecommunication Format (102-A2) |
Following is a list of information that may be required to process a claim.
|
FIELD |
DESCRIPTION |
|
Compound Code |
The Compound Code identifies the type of prescription as follows: 0 = Not specified. Use for DVS transactions. 1 = Not a compound - use when dispensing a prescription drug with an 11 digit NDC code. 2 = Compound - use when dispensing a compound drug. Please Note: 0 or 1 may be used for valid sickroom
supplies if you are using the NCPDP 5.1 format. Refer to sections 4.2 and 4.3
in the MMIS Pharmacy Provider Manual. The
837 Professional ASC X12N MUST be used for sickroom supplies
that are only billable under Category of Service 0442. (406-D6) |
|
Date
Prescription Written |
The Date the Prescription was written is entered in this field. The
Date Prescription Written must be no more than 60 days prior to the Date Filled for original scripts. For
Refills, the Date Prescription Written cannot be over 180 days old from the Date Filled. (414-DE) |
|
Days Supply |
The Days Supply is the estimated number of days that the prescription
should last. New York State does not accept a days supply greater than 366.
When the prescription's directions state "take as directed" (PRN),
it is strongly advised that 180 be entered as the days supply. (405-D5) |
|
Dispense As Written (DAW)/Product
Selection Code |
Acceptable values for the Dispense As Written (DAW)
code are as follows: 0 = No product selection 1 = Substitution not allowed by prescriber 4 = Substitution allowed - Generic Drug not in stock 5 = Substitution allowed - Brand Drug dispensed as a Generic 7 = Substitution not allowed - Brand Drug mandated by Law 8 = Substitution allowed - Generic Drug not
available in the Marketplace (408-D8) |
|
Eligibility
Clarification Code |
The Eligibility Clarification Code is used to indicate: · An eligibility override for Excess Income/Spenddown recipients when the spenddown has been met but eligibility has not been updated on file. · To resubmit a previously denied claim when a Client is a Resident of an In-State Skilled Nursing Facility or Health Related Facility which includes coverage for pharmacy services. When the Client has been discharged and the records still reflect residency within the Facility, the claim may be incorrectly denied. An override may be submitted which will result in a pend status, giving the local district time to update the Client’s file. Recognized value is: 2 = Override (309-C9) |
|
Fill Number |
The New/Refill Code values are as follows: 00 = New Prescription 01 = First Refill 02 = Second Refill 03 = Third Refill 04 = Fourth Refill 05 = Fifth Refill The maximum number of refills allowed is 5. This value cannot be
greater than the Number of Refills
Authorized. (403-D3) |
|
Number of Refills Authorized |
The Number of Refills Authorized is entered in this field. New York
State only allows a maximum of 5 refills. (415-DF) |
|
Other Coverage Code |
This field is used by the pharmacy to indicate whether or not the
patient has other insurance coverage. (308-C8) Valid entries NYSDOH are: 0 = Not Specified – Use for Medicare 1 = No Other Coverage Identified 2 = Other Coverage Exists, Payment Collected 3 = Other Coverage Exists, This Claim Not Covered. 4 = Other Coverage Exists, Payment Not Collected The
following codes if submitted will be cross-indexed as follows: 5 = Managed Care Plan –
Denial is equated to 3 6 = Other Coverage Denied – Not Participating
Provider is equated to 3 7 = Other
Coverage – Not in Effect at Time of Service is equated to 1 8 = Claim is Billing for Co-pay is equated to 2 (308-C8) |
|
Other Payor
Amount Paid |
For TPL: Enter the dollar amount of payments made by the other insurance. A
maximum of 9 amounts can be submitted. This field is used by the pharmacy to enter the dollar amount
received from a recipient’s other third party insurance company. Note: If other third party coverage exists but the claim
being submitted is not covered, enter zeros or blanks in this field. You may
also choose not to send this field if the primary carrier has denied the
claim. Refer to the chart in Section 2.5
on page 2.5.1 for information on the proper completion of this field. (431-DV) For MEDICARE: Enter a series of dollar amounts with the appropriate qualifiers to
identify the type of Medicare amount submitted. Refer to the Other Payer Amount Paid Qualifier (342-HC) below |
|
Other Payer Amount Paid Qualifier |
This code will qualify the other payer amount. Valid value for TPL
reporting is: 07 = Drug Benefit (342-HC) This code will qualify the other payer amount. Valid values for Medicare COB (Coordination of Benefits) reporting
are: 07 = Drug Benefit (used for Medicare Approved
Amount) 08 = Sum All Reimbursements
(used for Medicare Paid Amount) 99 = Other (1st 99 = Deductible Amount) 99 = Other (2nd 99 = Coinsurance Amount) 99 = Other (3rd 99 = Co-Payment Amount) (342-HC) |
|
Other Payer ID |
ID assigned to the
payer when submitting electronically. For TPL, enter any valid value that identifies the Third Party Payer. ID assigned to the payer when submitting Medicare COB claims. For Medicare use: 13 =
Medicare Part B. (340-7C) |
|
Other Payer Date |
Payment of denial Date
of the claim being submitted for coordination of benefits. (443-E8) |
|
Other Payer Amount Paid Count |
Other payer amount paid
count which is the count of other payer amount occurrences. (341-HB) |
|
Other Payer ID Qualifier |
Code qualifying the ‘Other Payer ID’. (340-7C) NYSDOH will process any valid value in conjunction with the Other
Payer ID. Examples would be, but not limited to the following: 01 =
National Payer ID 02 =
Health Industry Number (HIN) 03 = Bank
Information Number (BIN) 99 = Other For Medicare use: 99 =
Qualifies Medicare (339-6C) |
|
Other Payer Coverage Type |
Code identifying the Other Payer ID. (340-7C) 01 =
Primary 02 =
Secondary 03 =
Tertiary. (338-5C) |
|
Other Payer Reject Count |
Code identifying the number of third party denial codes. (471-5E) |
|
Other Payer Reject Code |
Enter the rejection code that was received from the primary payer. (472-6E) |
|
Patient Paid
Amount Submitted |
This field is used by the pharmacy to enter the dollar amount
collected as a spenddown from an excess income recipient. Note: If the spenddown was previously met but the
eligibility file has not yet been updated, enter zeroes in this field. Refer
to Section 2.13 on page 2.13.1
for additional information on this field. (433-DX) |
|
Primary Care Provider ID |
The Primary Prescriber is used to enter the 8 digit MMIS Provider ID
Number of the primary provider to which the recipient is restricted. This
field must be completed for a restricted recipient unless you are the primary
provider or the primary provider is indicated as the prescriber in field
411-DB. (421-DL) |
|
Primary Care Provider ID Qualifier |
This code will qualify the entry in field (421-DL). Primary Care
Provider Id field has a 8 digit Medicaid Provider Id number. Valid values
are: 05 = Medicaid (468-2E) |
|
Prior Authorization Number Submitted |
The Prior Authorization Number Submitted is used to enter a prior
approval number. The format for this field is: an 8 digit prior approval
number and then three zeroes. Refer to Section
2.11 on page 2.11.1 for additional information on this field. (462-EV) |
|
Prior Authorization Type Code |
This code will specify co-pay exemption or clarify a Prior
Authorization request or submission. Valid values are: 0 = Not specified 1 = Prior Authorization 4 = Exemption from co-pay (461-EU) |
|
Prescriber ID |
The Prescriber ID is the Ordering Provider who wrote the
prescription. Either the ordering provider's MMIS Provider ID number or
license type and license number must be entered. Refer to MEVS Denial code
056 in Table 2 on page 10.0.1 for further
clarification. (411-DB) |
|
Prescriber Id Qualifier |
The code entered will qualify the entry in the Prescriber Id (411-DB)
field as either a MMIS Provider Id or a State License number. Valid values
are: 05 = Medicaid 08 = State License (466-EZ) |
|
Prescription/Service Reference Number |
The Prescription Number is assigned by the pharmacy. Reference number
assigned by the provider for the dispensed drug / product and/or service
provided. (402-D2) |
|
Prescription/Service
Reference Number Qualifier |
Indicates the type of billing submitted. Valid Values are: 1 = Rx Billing NYSDOH only supports prescription billing. (455-EM) |
|
Product/Service
Id Number |
The NDC Number is the 11 digit National Drug Code identifying the dispensed drug. When using compounds use code 99999999999. (407-D7) |
|
Product/Service Id Qualifier |
The Product/Service Id Qualifier is used to identify the Product Type
dispensed. This field must contain a HCPCS "09" when the item
dispensed is a product supply item (sections 4.2 and 4.3
in the MMIS Pharmacy Provider Manual), or for item codes requiring a DVS
number which were published in a list. 09 = HCPCS 03 = NDC (436-E1) |
|
Reason for
Service Code |
The DUR Conflict Code is used to indicate an override for a DUR reject of a previously entered claim.
Acceptable values are: TD = Therapeutic Duplication DD = Drug to Drug Interaction (439-E4) |
|
Result of
Service Code |
The DUR Outcome Code is used to indicate the action taken by the
pharmacist, and is required for a DUR override.
Acceptable values are: 1A = Filled as is, false positive 1B = Filled, Prescription as is 1C = Filled with Different Dose 1D = Filled with Different Directions 1E = Filled with Different Drug 1F = Filled with Different Quantity 1G = Filled with Prescriber Approval (441-E6) |
|
Submission Clarification Code |
The Submission Clarification Code is used to indicate a Utilization
Threshold override and replaces the use of the SA Exception Code. Following
are the recognized values: 00 = Not Specified 01 = No Override 02 = Other Override - use to replace SA Exception Code P (pending an override) 07 = Medically Necessary - use to replace SA
Exception Code J (Immediate Urgent
Care) & L (Emergency). Note: These are the only values used for UT Override by
NYSDOH when using the NCPDP format. Any other value entered in this field
will be ignored. (420-DK) |
|
Quantity
Dispensed |
The Quantity Dispensed is the total number of Metric Units dispensed
for the prescription. (442-E7) |
|
Usual and Customary Charge |
The Usual and Customary Charge is used to enter the amount charged
for the prescription. (426-DQ) |
The information that is received from the New York State Department of Health (DOH) Pro-DUR/ECCA system will vary depending upon whether the claim has been accepted or rejected. A separate response will be received for each claim submitted. For example, if three claims are submitted at a time, three responses will be returned from Pro-DUR/ECCA.
The NCPDP field numbers are shown in parenthesis at the end of the description for each field.
Following is a description of the information returned from Pro-DUR/ECCA for each request that is sent.
|
FIELD |
DESCRIPTION |
|
Header Response
Status |
An A (Accepted) will be returned if the information in the transmission is valid. An R (Rejected) will be returned if the information in the transmission is invalid. Further clarification of the reject will be indicated by NCPDP Reject codes and in the Message Area. Note: When an R is returned in the Header Response Status, all of the claims submitted on this request transaction will be rejected. (501-F1) |
Following is a description of the information that will be returned from Pro-DUR/ECCA for each claim sent.
Note: The following field descriptions are in alphabetical order and not necessarily the order in which they appear in the response.
|
FIELD |
DESCRIPTION |
|
Additional Message
Info |
The Additional message area,
in the NCPDP format, is used to return additional MEVS information about your
request transaction. Your system may separate this information to clearly
identify the contents of this additional message. However, some systems may
display this message as it is returned in the NCPDP format. The following
information is returned in the Additional Message: MEVS Accepted or Pending Code Utilization Threshold/Post & Clear Code Maximum Per Unit Price Co-Payment Code Co-Pay Met Date DVS Reason Code Medicare
Coverage HIC Number Insurance Carrier Codes Insurance Coverage Codes Indication of Additional Coverage Restriction Information - Exception Codes Dispensing Validation System Number (526-FQ) Please refer to Chart B
on page 8.0.3 for an example of the Additional Message. The following information is returned in the
Message field for rejected claims (when Claim
Response = R): MEVS Accepted, or Denial Code Rx Denial Code Utilization Threshold/Post & Clear Code DVS Reason Code Please refer to Chart C for an example of the Message. (526-FQ) |
|
Amount of Copay/ Coinsurance
|
The amount of co-pay due for the entered NDC or HCPCS (NY Product
Supply Code) will be returned in the Amount of Copay/Coinsurance if the
recipient has not met their co-pay or is exempt. (518-FI) |
|
Anniversary Month |
The Anniversary Month found in the Message Text is the beginning month of the benefit year under the
Utilization Threshold program. (504-F4) |
|
Authorization Number |
The authorization number is the 9 digit invoice number returned if
ECCA was requested and all edits were passed. This is the invoice number that
will appear on your remittance statement from the eMedNY contractor. Please
Note: NO CLAIM TO FA will be returned if the claim is captured but cannot be
processed for adjudication. Below are a few examples of when this will occur: •
Original claims over
90 days old. •
Processor Control
Number blank or missing. If a claim is captured but cannot be processed for adjudication, it
must be billed via paper, on magnetic media or Electronic Batch Dial-Up.
(503-F3) |
|
Category of Assistance |
Category of Assistance Code returned within the Message Text: S = SSI * = No
valid category of assistance is available (504-F4) |
|
Transaction Response Status |
This is the status for each claim that was submitted. A "C" indicates that the claim is accepted and/or pending, and
an "R" indicates that it is rejected. A separate Claim Response
Status will be received for each claim submitted on your request (1 - 4).
Refer to the Reject Codes, the MEVS Denial Code, the Rx Denial Code, the Utilization Threshold/Post & Clear
Code, and the Dispensing Validation Reason Code to determine why an
"R" is returned in the Claim Response Status. If a "C" is returned, the Authorization Number field must be
checked to determine if the claim has been electronically captured for
adjudication. The MEVS Pend Response Code Table should also be checked to see
if the claim is pending. (112-AN) |
|
Clinical Significance |
Clinical Significance returned within the DUR Response area indicates
how critical the conflict is. This value reflects the severity level assigned
to a contraindication. Refer to DUR
Processing Section for a list of clinical significance codes and their
meanings. (528-FS) |
|
Co-Payment Code |
The Co-Payment Code returned within the Additional Message area provides the status of co-payment for this claim. (526-FQ) |
|
Co-Payment Met Date |
The Co-Payment Met Date returned within the Additional Message area identifies the date the recipient has met this year's
co-payment requirement. (526-FQ) |
|
County Code |
The two-digit code for the county of fiscal responsibility for the
recipient is provided within the Message
Text. Refer to the list of county codes in the Codes section of the MEVS
Manual. (504-F4) |
|
Database Indicator |
The Database Indicator returned within the DUR Response area is
always 1 to indicate that First
DataBank is the source of the DUR database. (532-FW) |
|
Dispensing Validation System Number |
The eight digit DVS Number (prior approval) will be returned in the Additional
Message area if the DVS transaction is accepted. The number will be
automatically entered on your ECCA claim for adjudication processing. If you
did not submit the claim for ECCA and are billing manually, this number must
be put on your claim form. (526-FQ) |
|
Dispensing Validation System Reason Code |
The three-digit code indicating either the accepted or rejected
status of the DVS request is returned within the Additional Message area. Refer to Table 9 for the codes and descriptions. (526-FQ) |
|
Reason for Service Code |
The Reason for Service Code returned within the DUR Response area will be generated and sent back to the pharmacy when a DUR conflict is detected. Refer to DUR Processing section for further clarification. The following values may be returned. TD = Therapeutic Duplication DD = Drug-Drug Interactions DC = Inferred Drug Disease Precaution PG = Drug Pregnancy Alert PA = Drug Age Precaution LD = Low Dose Alert HD = High Dose Alert (439-E4) |
|
Exception Codes |
Up to four Exception Codes may be returned within the Additional Message area. These codes
indicate special eligibility circumstances and can be found in the Codes
section of the MEVS Provider Manual. (526-FQ) |
|
Free Text |
The Free Text returned within the DUR Response area contains
information to assist the pharmacist in further identifying the DUR conflict.
Please refer to the DUR Processing section.
(544-FY) |
|
HIC Number |
The HIC Number returned within the Additional Message area is the Health Insurance Claim number for
Medicare. (526-FQ) |
|
Indication of Additional Coverage
|
A ZZ in the Indication of Additional Coverage,
returned within Additional Message
area, indicates that the recipient has more than two insurance carriers. You
must call the Provider Services Department at 1-800-343-9000 to obtain
complete information. (526-FQ) |
|
Insurance Carrier Codes |
Up to two Insurance Carrier Codes are returned within the Additional Message area to provide
the codes for insurance carriers. (Also, see Insurance Coverage Codes). (526-FQ) |
|
Insurance Coverage Codes |
Up to two sets of Insurance Coverage Codes are returned within the Additional Message area. These
correspond one for one to the Insurance
Carrier Codes and indicate the scope of benefits. Refer to the Codes
section of the MEVS Provider Manual for a description of the Insurance
Coverage Codes. (526-FQ) |
|
Maximum Per Unit Price |
The Maximum Per Unit Price returned within the Additional Message Area is the per unit amount
on New York State’s Drug File. The price is the maximum reimbursable unit
price amount. The dollar amount
returned to you in your response does not indicate the amount of payment you
will receive. (526-FQ) |
|
Medicaid Number |
The Client's Identification Number (CIN) is provided within the
Message
Text. (504-F4) |
|
Medicare Coverage |
The Medicare Coverage code is returned within the Additional Message area and indicates
the type of Medicare coverage. A = Recipient has only Part A Medicare coverage (inpatient hospital). B = Recipient has only Part B Medicare coverage (outpatient). AB = Recipient has both Part A and Part B Medicare coverage. ABQMB = Recipient
has Part A and Part B Medicare coverage and is a Qualified Medicare
Beneficiary (QMB). If a recipient’s eligibility code is 09 (Medicare
Coinsurance/Deductible), Medicaid will only reimburse for the Medicare
coinsurance/deductible if Medicare approves the drug or item being
dispensed. Since the majority of drugs are not covered by Medicare,
Medicaid would not be making payment in most cases. Therefore, the DUR system
has been programmed to reject this type of claim (Table 2 code 105). In the
rare case that Medicare does approve the drug, the claim can be manually
submitted to the eMedNY contractor for payment. If the recipient has full
Medicaid coverage (coverage code 01) and is QMB, the claim will not be
rejected but will be captured and if ECCA was opted, processed for
adjudication. (526-FQ) |
|
MEVS Accepted Code |
The MEVS Accepted Code returned within the Additional Message area indicates the type of
Medicaid eligibility the recipient has. Refer to Table 1 on page 9.0.1 for a list of values
and meanings. (526-FQ) |
|
MEVS Denial Code |
The MEVS Denial Code returned within the Additional Message area indicates the type of MEVS error for rejected transactions.
Refer to Table 2 on page 10.0.1 for a list
of values and meanings. (526-FQ) |
|
A Message Text area returned in the NCPDP format is
used to provide MEVS information about your requested transaction. Your
system may separate this information to clearly identify the contents of this
message. However, some systems may display this message as it is returned in
the NCPDP format. The following information is returned in the Message field
for accepted claims (when Claim
Response = C): Medicaid
Number County Code Anniversary
Month Patient
Gender Code Year of
Birth Category of
Assistance Re-certification
Month Office
Number Service Date Please refer to Chart A on page 8.0.2 for an example of the Message. (504-F4) |
|
|
Office Number |
The Office Number returned
within the Message Text represents the New York City
office code. Refer to the Codes section of the MEVS Provider Manual for a list of
valid office codes. (504-F4) |
|
Other Pharmacy Indicator |
The Other Pharmacy Indicator
returned within the DUR Response area indicates the source of the
previous prescription that forms the basis for the conflict with the
present prescription. The following values may be returned. 1 = Your Pharmacy 3 = Other Pharmacy (529-FT) |
|
Other Prescriber Indicator |
The Other Prescriber Indicator returned within the DUR Response area compares the Prescriber of the current prescription to the Prescriber of the previously filled conflicting prescription. The following values may be returned: 0 = Not Specified 1 = Same Prescriber 2 = Other Prescriber (533-FX) |
|
Pend Reason Code |
The Pend Reason Code returned
within the Additional Message
Area indicates that the claim has passed all other online adjudication
edits but has been pended for one of the reasons listed in Table 10 (page 15.0.1). Refer to Section 15.0 on page
15.0.1 for values and descriptions. The Table 10 (page 15.0.1) reason code will be returned in the
same field positions that a Table 1 (page 9.0.1) Accepted Code is normally returned
(526-FQ) field. Consequently, when the return of a Table 10 (page 15.0.1) Pend Code is warranted, a Table 1 (page
9.0.1) Accepted Code will not be returned. (526-FQ) |
|
Previous Date of Fill |
The Previous Date of Fill
returned within the DUR Response area is the date that the previous
prescription was filled. (530-FU) |
|
Quantity of Previous Fill |
The Quantity of Previous Fill
returned within the DUR Response area is the quantity of the
previously filled prescription. (531-FV) |
|
Recertification Month |
The Recertification Month
returned within the Message Text is
the
month the recipient is due for recertification. (504-F4) |
|
Reject Codes |
A maximum of 20 Reject Codes
could be returned if the Claim Response Status is "R" (Reject). Refer to NCPDP Reject Code list on page 16.0.1 for values. (511-FB) |
|
Rx Denial Code |
The Rx Denial Code returned
within the Additional Message
area provides prescription
related reject reasons. Refer to Table 7 on page 12.0.1 for possible values.
(526-FQ) |
|
Service Date |
The Service Date returned
within the Message Text is the
same as the Date Filled (or dispensed), entered on your
transaction. (504-F4) |
|
Patient Gender Code |
Valid patient gender Codes returned within the Message Text are: F = Female M = Male U = Unborn (504-F4) |
|
Utilization
Threshold/ Post and Clear |
The Utilization Threshold/Post
& Clear codes indicate the status of the UT/P&C service authorization
requests. Refer to Table 8 on page 13.0.1 for further clarification. (526-FQ) |
|
Year
of Birth |
The Year of Birth returned
within the Message Text shows the
century
and year of the recipient's birth. Example: 1980 will appear as
980. (504-F4) |
This section describes the use of reversal transactions in the New York State Pro-DUR/ECCA system. A reversal transaction is used to cancel or reverse a previously submitted claim that was approved by the Pro-DUR/ECCA system. A reversal can now be used to void out a paid claim submitted via paper, magnetic media or Batch Pharmacy Dial-Up. Reversal transactions can be submitted online up to two years from the service date.
Reversal transactions can only cancel one claim at a time. For example, if four claims were submitted and approved on a single transaction request, four separate reversal transactions would be needed to cancel the entire transaction.
The primary matching values used to determine which claim is being canceled are the Service Provider Id (201-B1), Prescription/Service Reference # (402-D2), and Date of Service (401-D1), which were submitted on the original claim. If the reversal is approved, code 021 is returned in the MEVS Accepted Code. If no match is found for the reversal, code 045 (No Authorization Found) is returned in the MEVS Denial Code.
The following fields are required for a reversal transaction. Please see the Pro-DUR/ECCA Input Information section for a description of these fields.
BIN Number
Version/Release
Number
Transaction
Code (B2)
Service
Provider Id
Service
Provider Id Qualifier
Date
of Service
Prescription/Service
Reference #
Prescription/Service
Reference # Qualifier
Processor
Control Number (if a paid claim is
being reversed)
The following information is returned if the cancel is accepted.
Transaction Response Status (A)
Authorization Number (The invoice number of the original claim will be returned in the response.)
MEVS Response Code (021)
The following information is returned if the cancel was denied.
MEVS Denial Code (R)
Rx Denial Code
Reject Codes (up to 10)
NCPDP Reversals can be submitted for service dates up to two years old as long as the previous transaction (either ECCA, non-ECCA, or claims submitted via paper, magnetic media or Batch Pharmacy Dial-Up) was submitted directly to the eMedNY contractor, or the transaction was submitted to eFunds no longer than 90 days prior to the eMedNY contractor takeover of the MEVS system.
By submitting a reversal via NCPDP format, you can either: reverse a previous NCPDP transaction, or use the NCPDP reversal to void a claim sent via paper, magnetic media or Batch Pharmacy Dial-Up. If a non-capture transaction (NO CLAIM TO FA) is being reversed, the action taken by the claims processing system is contingent on if the subsequent paper, magnetic media or Batch Pharmacy Dial-Up claim was approved during the interim.
If a paper, magnetic media or Batch Pharmacy Dial-Up claim was approved for payment during the interim, the paper, magnetic media or Batch Pharmacy Dial-Up claim will be voided, and any units used by the claim will be restored to its applicable service authorization or prior approval. The service authorization and prior approval will remain available for future use until the record becomes inactive.
If a subsequent paper, magnetic media or Batch Pharmacy Dial-Up claim has not been approved for payment during the interim, the non-capture transaction will be reversed, and any applicable service authorization or DVS prior approval generated as a result of submitting the non-capture transaction will be cancelled. When cancelled, the authorizations and approvals previously generated are no longer useable.
When reversing a previously submitted ECCA transaction that was captured for payment, if approved, the reversal will cancel any service authorization or DVS prior approval generated by the original transaction.
If you need to
reverse a previously paid ECCA, paper, or magnetic media claim online, you must
complete the processor control number field on the reversal transaction. If
omitted, your reversal will be rejected for response code 323 (refer to Table 2 codes on page 10.0.1). If you need to
reverse a non-ECCA claim, then you may choose to forego entering your processor
control number.
The following charts are used to illustrate various types of messages you can receive from your transactions. The charts are shown as to content of data. A single chart does not reflect the entire message you will receive in a single response.
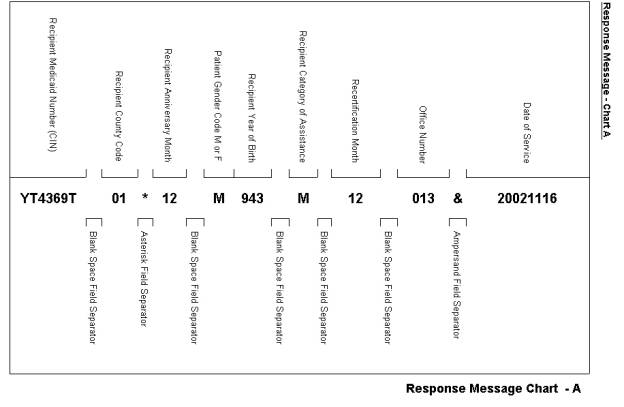
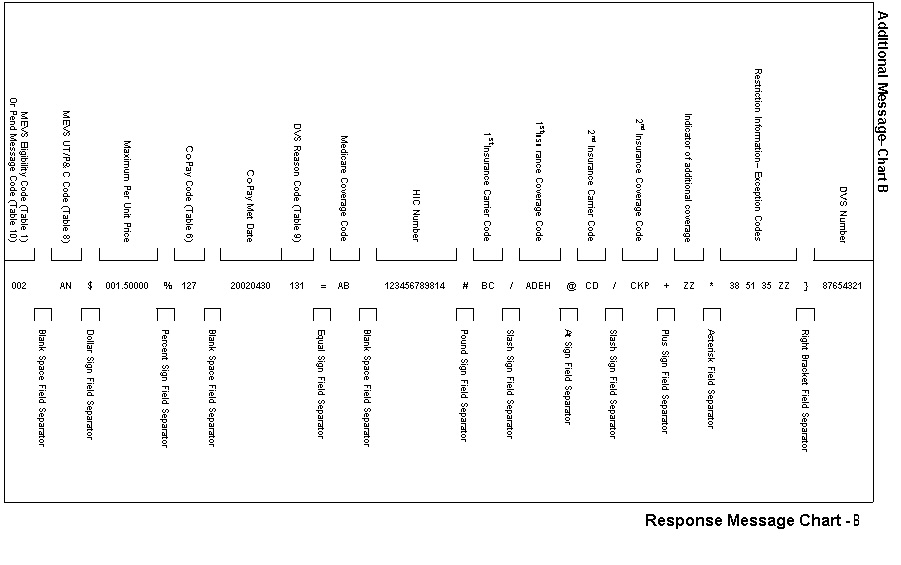
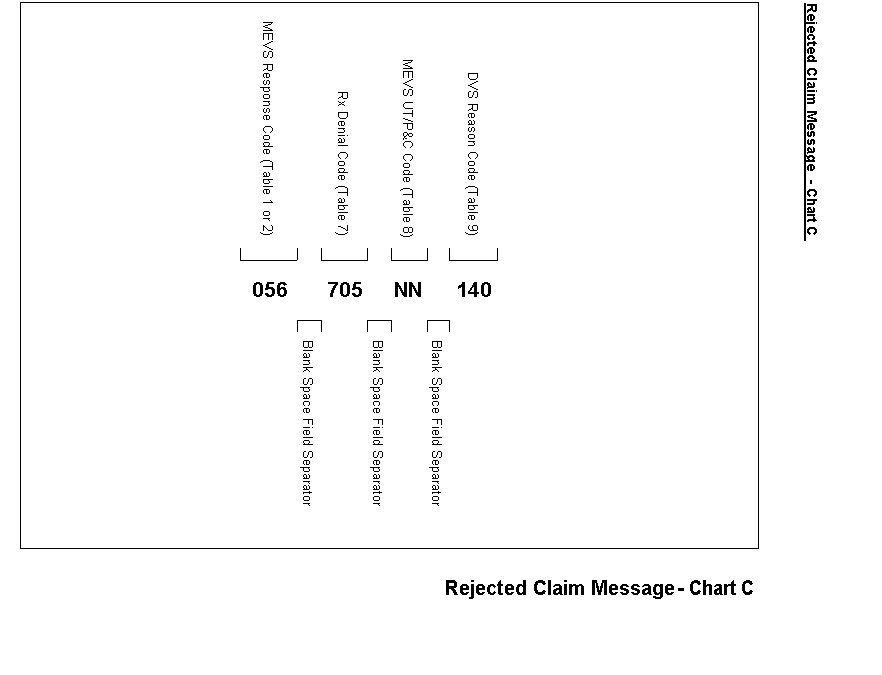
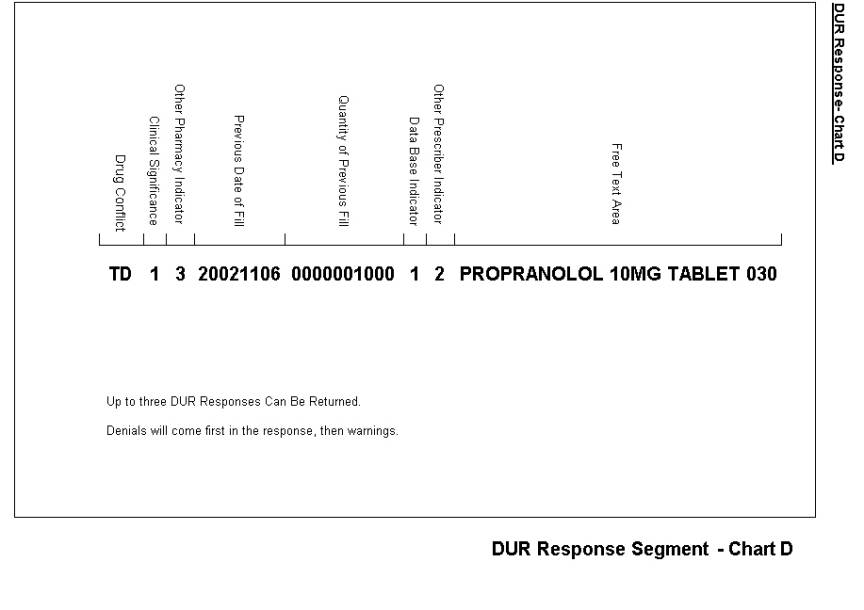
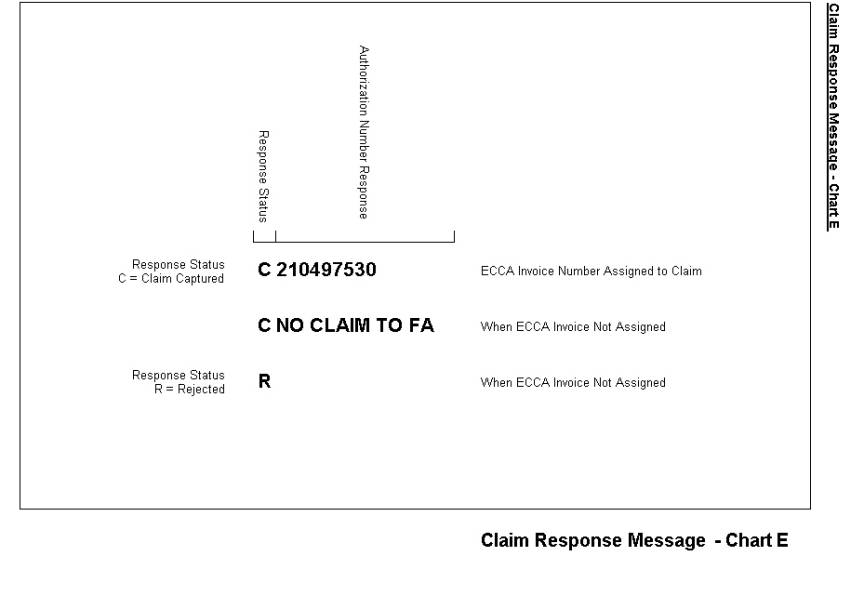
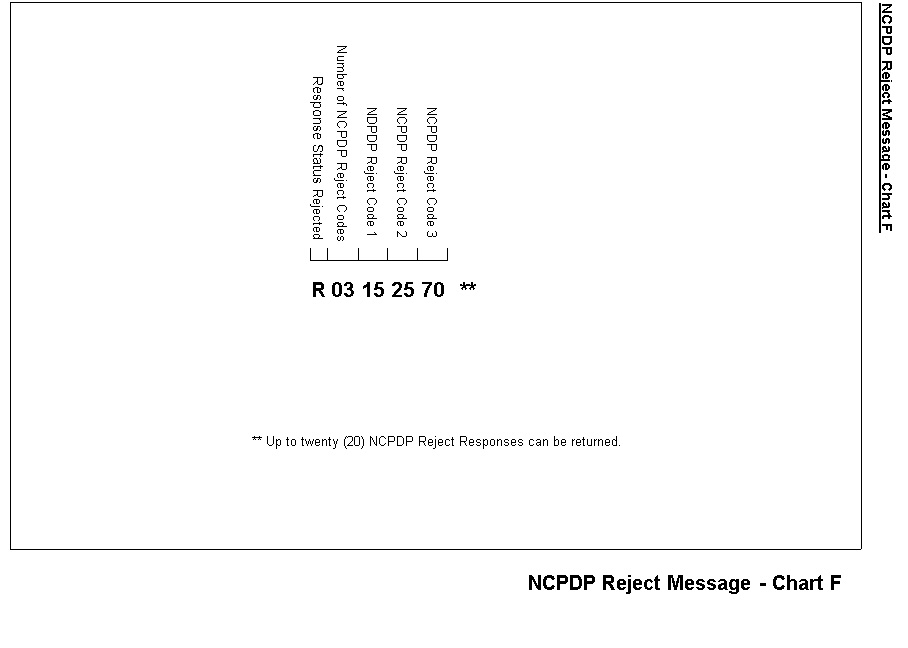
All of the Table 1 codes (except 017 and 021) indicate the type of Medicaid eligibility for the recipient. If the recipient is Medicaid eligible, a Table 1 code will be returned on each claim transaction even if the transaction is rejected for other reasons. (i.e.: Utilization Threshold, DUR Denial, etc.). An exception to this is if the transaction is rejected for header field errors (Code 999 found in Table 2 on page 10.0.1) and is not processed through the eligibility modules or an invalid Medicaid ID or sequence number is entered. Another exception is when a pend reason code from Table 10 is warranted in the response. Table 1 codes are eligibility codes. There are no existing comparable NCPDP codes that are returned with these codes.
Code 017 does not indicate Medicaid eligibility but denotes a recipient enrolled in the Family Health Plus Program.
Code 021 is not an eligibility status code. It is returned if your transaction to cancel a previously accepted claim has been accepted.
|
Code |
Description |
|
002 |
MA Eligible |
|
003 |
Eligible Only
Outpatient Care |
|
005 |
Eligible Capitation
Guarantee Only |
|
006 |
Eligible PCP |
|
007 |
Emergency Services Only |
|
008 |
Presumptive Eligible
Long-Term/Hospice |
|
009 |
Medicare Coinsurance
Deductible Only |
|
010 |
Eligible Except Nursing
Facility Services |
|
013 |
Presumptive Eligibility
Prenatal A |
|
014 |
Presumptive Eligibility
Prenatal B |
|
015 |
Perinatal Family |
|
016 |
MA
Eligible-HR-Utilization Threshold |
|
017 |
Family Health Plus
Services Only |
|
018 |
Family Planning
Services Only |
|
021 |
Record Canceled –
Cancels a Previously Accepted Claim |
|
034 |
Community Coverage with
Community Based Long Term Care |
|
035 |
Community Coverage
without Long Term Care |
|
036 |
Outpatient Coverage
with Community Based Long Term Care |
|
037 |
Outpatient Coverage
without Long Term Care |
|
038 |
Outpatient Coverage
with No Nursing Facility Services |
All of the following codes are MEVS Denial Codes. Their presence in your response area means the entire transaction has been rejected. If a MEVS Denial Code has a comparable NCPDP Reject Code, both codes will be returned. If there is no comparable code, then NCPDP code 85, "Claim Not Processed" is returned along with the MEVS Code. In those cases, the MEVS Denial Code will further qualify the reason for the claim being rejected. The following chart indicates the relationship between the MEVS Denial Code and any comparable NCPDP Reject Code, if one applies.
Code 999 will be returned if any invalid data is entered in the NCPDP required header fields. For example, an entry of 05 in the Transaction Code field will result in an MEVS Denial Code 999 being returned since it exceeds the number of claims authorized to be sent in a transaction. Also included is a description and relevant comments about the code.
|
MEVS CODE |
DESCRIPTION |
NCPDP CODE |
DESCRIPTION |
|
001 |
Not MA Eligible |
65 |
Patient is Not Covered |
|
030 |
Expired Card |
07 |
M/I Cardholder ID
Number |
|
031 |
Invalid Card Status |
07 |
M/I Cardholder ID
Number |
|
033 |
Non-Current Card |
07 |
M/I Cardholder ID
Number |
|
045 |
No Authorization Found |
87 |
Reversal Not Processed |
|
050 * |
Alternate Access Not
Allowed |
** |
|
|
051 |
Invalid Provider Number |
05 |
M/I Pharmacy Number |
|
052 |
Provider Not on File |
50 |
Non-Matched Pharmacy
Number |
|
053 |
SSN Access Not Allowed |
07 |
M/I Cardholder ID
Number |
|
054 |
Provider Cannot Access
by Account Type |
** |
|
|
055 |
Provider Not Eligible |
** |
|
|
056 * |
Re-enter Ordering
Provider Number |
25 |
M/I Prescriber ID |
|
059 * |
Invalid License Type |
25 |
M/I Prescriber ID |
|
061 * |
Invalid Access Number |
07 |
M/I Cardholder ID
Number |
|
062 * |
Invalid Medicaid Number |
07 |
M/I Cardholder ID
Number |
|
063 * |
Invalid Sequence Number |
08 |
M/I Person Code |
|
065 |
Recipient Not on File |
52 |
Non Matched Cardholder
ID |
|
066 |
Disqualified Ordering
Provider |
25 |
M/I Prescriber ID |
|
067 |
Deceased Ordering
Provider |
25 |
M/I Prescriber ID |
|
068 |
Invalid Ordering
Provider |
25 |
M/I Prescriber ID |
|
071 |
Invalid Date |
15 |
M/I Date of Service |
|
092 |
Invalid Specialty Code |
05 |
M/I Pharmacy Number |
|
100 * |
Invalid Referring
Provider Number |
35 |
M/I Primary Care
Provider Id |
|
101 * |
Restricted Recipient No
Auth |
35 |
M/I Primary Care
Provider Id |
|
103 |
No Coverage: Pending
Family Health Plus |
65 |
Patient Not Covered |
|
104 |
No Coverage: Excess
Income |
65 |
Patient Not Covered |
|
105 |
QMB Requires Medicare
Approval |
65 |
Patient Not Covered |
|
118 * |
MCCP Recipient No Auth |
35 |
M/I Primary Care
Provider Id |
|
300 |
Service Date Prior to
Birthdate |
09 |
M/I Birthdate |
|
302 |
Provider Ineligible
Service on Date Performed |
** |
|
|
303 |
Prior Approval
Indicated Denied/Rejected by NYS |
EV |
M/I Prior Authorization
Number Submitted |
|
304 |
Recipient ID Unequal to
Prior Approval File |
EV |
M/I Prior Authorization
Number Submitted |
|
305 |
Child Care Recipient –
Bill Agency |
** |
|
|
307 |
Prior Approval Units or
Payment Amount Exceeded |
** |
|
|
308 |
Service Date Not Within
Prior Approval Range |
** |
|
|
309 |
Claim Type Unequal to
Prior Approval Record Class |
** |
|
|
312 |
Pregnancy Indicated –
Invalid for Recipient Sex or Age |
** |
|
|
313 |
Provider Reimbursed for
Medicare Only |
** |
|
|
314 |
Recipient Not QMB,
Services Not Reimbursable |
** |
|
|
315 |
Recipient Not Medicare,
Services Not Reimbursable |
** |
|
|
316 |
Claim Previously Paid
Using Another Provider Number |
** |
|
|
318 |
Prescribing Provider
License Not in Active Status |
25 |
M/I Prescriber ID |
|
320 |
Other Insurance
Information Inconsistent |
DV |
|
|
321 |
Pharmacy Service
Included In Out-of-State Facility Rate |
** |
|
|
322 |
Online
Adjustments/Rebills Not Allowed For DVS Items/Drugs |
** |
|
|
323 |
Processor Control
Number Needed for Rebill/Reversal of Paid Claim |
** |
|
|
324 |
The system or file
necessary to process the transaction is currently unavailable. |
92 |
System Unavailable |
|
325 |
Pharmacy Service
Included in In-State Facility Rate |
** |
|
|
700 * |
Year of Birth Not Equal
to File |
09 |
M/I Birthdate |
|
701 |
Sex Not Equal to File |
10 |
M/I Patient Gender Code |
|
702* |
ECCA Not Allowed |
81 04 |
Claim
too Old M/I Processor Control
Number |
|
703 * |
Invalid PIN |
04 |
M/I Processor Control
Number |
|
704 * |
Invalid ETIN |
04 |
M/I Processor Control
Number |
|
999 |
Header Field Error |
*** |
|
* For further explanation and examples of error conditions refer to Table 2 Error Chart
** NCPDP equivalent reject code does not exist. Code 85 "Claim Not Processed" will be returned.
*** Several Different NCPDP Reject Codes could be returned with MEVS Code 999. These Reject Codes will indicate which header field is in error.
TABLE 2 ERROR CHART (Rev. 10/04)
Key: b = Blanks/Spaces
Left Justify = Begin in First Position on Left
|
MEVS CODE |
NCPDP CODE |
EXAMPLES OF CORRECT ENTRY |
COMMON ERRORS BEING MADE / COMMENTS |
|
050 Alternate
Access not allowed |
None |
None - No entry made |
1. In order to access the DUR/ECCA online system you
must choose an alternate access method. 2. Code 050 will be returned if your provider number
has not been updated with your selected access method on the eMedNY
contractor’s production file. 3. In order to be updated on the production file, you
must have: A) Notified the eMedNY contractor of your alternate
access method. B) Signed the contract and sent it to the eMedNY
contractor. C)
Signed the contract
and submitted your check to your switch company if you chose to transmit
through a switch. The switch must then send an approval to the eMedNY
contractor before your number will be updated on production. |
|
053 SSN Access Not Allowed |
None |
None – 9 digit entry not
allowed |
Card holder ID (302-C2)
field has only two acceptable formats: 1. Eight
position alpha/numeric Medicaid Client Number (CIN) OR 2. Thirteen-digit Access
Number without the six-digit ISO # prefix |
|
054 Provider Cannot Access by Account Type |
None |
None – No entry made |
If you submit a
transaction via an access method other than the method assigned to your
provider number on the production file, code 054 will be returned. For
example, if your provider number is on the file as going through a switch
company and a transaction is sent using a second switch company that is not
on your file, your transaction will be rejected. |
|
056 or 059 Reenter Ordering Provider Number or Invalid License Type |
25 M/I
Prescriber ID |
0100567892 (NYS
Physician) 290F654938 (Nurse
Practitioner) 00240588 (8
digit MMIS Provider ID for enrolled prescriber) 11NJ456193 (Out
of State Physician from New Jersey). 250U452749 (Optometrist) |
1. The Prescriber ID field length is 10. The Prescriber's License
type must be in the first two positions, followed by either two zeroes or two
alpha (out of state) followed by the 6 digit license number. The Prescriber
ID Qualifier must be equal to 08 when submitting a license number. An 8 digit
provider number must be left justified, space filled. The Prescriber ID
Qualifier must be equal to 05. Note: When entering a license number,
the last six positions of the entry should be the actual numeric license
number. If the license number does not contain six numbers, zero fill the
appropriate positions preceding the actual license number. For example, an
entry for an Optometrist whose license number is U867 would be 250U000867. 2. Some incorrect entries being received are: A)
567892:
License number only B)
00567892:
License number without License Type. C)
0156892:
License Type, License Number without zeroes or 2 alpha in between. D)
E)
DEA
Number: Some software packages are sending the physician's DEA numbers
instead of the license number. 3.
Nurse Practitioners: A nurse practitioner may have several different
license numbers because the State Education Department issues them a license
for each specialty for which they are certified. Not All Nurse Practitioners
are licensed to prescribe drugs. A nurse practitioner who is licensed to
prescribe will have the letter "F" preceding the 6 digit license
number. This is the license number that must be used when submitting your
transaction. The license type 29 followed by 0F and the 6 digit number is the
only correct entry for nurse practitioners’ license numbers. 4. Optometrists: An optometrist who is licensed to prescribe will
have the letter ‘U’ or ‘V’ preceding the six -digit license number. The
license type 25 followed by ‘OU’ or ‘OV’ and the six- digit number are the
only correct entries for optometrists’ license numbers. |
|
061 Invalid
Access Number 062 Invalid
Medicaid Number. |
07 M/I
Cardholder ID Number |
2631578424139 (13
digit access number found on recipient's Medicaid card) LZ00083W (CIN Number) |
1. The entry in the Cardholder ID field must contain
either the recipient's 13 digit access number or their 8 character alpha
numeric CIN number. Both must be left justified, space filled. 2. The most common error being received that causes
code 061 to be returned is an entry of 8 numeric digits in the Cardholder ID
field. Check your software to make sure the alpha characters in the CIN
number are not being converted to numeric values. 3. Rejections also occur when either number is not left
justified. 4. Code 062 is returned when the number entered cannot
be found on the file. |
063 Invalid
Sequence Number |
08 M/I
Person Code |
03 (2
digit sequence number) 12 (2
digit sequence number) |
1. The recipient's 2 digit sequence number is required
on each transaction. The sequence number can be found on the recipient's
Medicaid card. 2. Our format requires the 2 digit sequence number to
be placed in the 3 digit Person Code field. The number must be left justified
and space filled. We have learned that some software packages have the number
placed in a different field, which is fine as long as it is sent to the
eMedNY contractor in the Person Code field. 3. Some incorrect entries being received are: A) Person Code field is blank B) Sequence number is not left justified. C)
Sequence number
transmitted does not match the most current number on the eMedNY contractor’s
file. A new sequence number is issued each time a recipient receives a new
card. |
|
100 Invalid
Referring Provider Number 101 Restricted
Recipient No Auth 118 MCCP
Recipient No Auth |
35 M/I
Primary Care Provider Id |
00240588 (8
digit MMIS identification number of the provider to which a recipient is
restricted). |
1. If a recipient is restricted, the Primary Care
Provider field must contain the 8 digit MMIS Number that the recipient is
restricted to. The provider number is the only valid entry. An entry
in this field is in addition to an entry in the Prescriber ID
field. The entry must be left justified and space filled. The Primary Care
Provider ID Qualifier must have a value of 05 when this field is entered. 2. Some incorrect entries being received are: A) B) 00240588bA: Eight digit MMIS Provider number left
justified but followed by a space and an alpha character. C) Field is blank and recipient is restricted. D) Field contains the same provider number that is
being sent in the Prescriber ID field and recipient is not restricted to that
provider. E)
Field contains a
license number. |
|
700 Year
of Birth not equal to file. |
09 M/I
Birthdate |
19490228 (Century,
Year, Month, Day) |
The Date of Birth field
requires an 8 digit entry, which includes the Century of the recipient's
birth. The majority of your software packages only require you to enter the
birth year and the software is automatically sending 19 as the Century. This
has caused some rejections when the recipient was born in the 18th Century.
When this occurs, you need to contact your software company. |
|
702 ECCA
Not Allowed |
81 Claim Too Old |
20010601 (Century,
Year, Month, Day) |
1. The date
filled requires an eight-digit entry, which includes the century of the date
filled. The eMedNY contractor will only accept fill dates up to two years old
via NCPDP for rebills and reversals. This reject will be returned for any
rebill or reversal with a fill date over two years old. |
|
|
04 M/I Processor Control Number |
Y (Yes) |
2. The first
position of the Processor Control Number must equal ‘Y’ to indicate the
provider has read and attests to the data in the Certification Statement on page 19.0.3. |
|
703 Invalid
PIN 704 Invalid
ETIN |
04 M/I
Processor Control Number |
YTG1234QBK (Certification, Initials, PIN, ETIN) |
1. If you
wish your transaction to be electronically captured, the Processor Control
Number field must be completed. Correct completion of this field alerts the
online system to capture an accepted claim transaction for adjudication. 2. The
reject denial code 703 will be returned if: A.) You have not
submitted the PIN selection form to the Department of Health. B.) The PIN number has
not been added to your provider file record at the eMedNY contractor. C.) The PIN number
transmitted does not match the number selected, which was added to your
provider file record. 3. The
reject denial code 704 will be returned if: A.) You have not applied for and/or submitted your ETIN number on a notarized certification statement to the eMedNY contractor. B.) The
ETIN transmitted does not match the ETIN submitted on the certification
statement, which was added to the ETIN file. 4. Some
software has hard coded the ETIN of the billing service into this field. If
that ETIN was not on the certification statement, the transaction will
reject. |
|
705 NDC/APC
Not Covered |
70 Product/Service
Not Covered 77 Discontinued
Product/Service Id Number |
00074738601 (11
digit NDC Code) |
1. The Product/Service Id field entry must contain an
11 digit numeric NDC code. 2. Some common errors being received are: A) NDC field is blank - software is not pulling code
off of your drug file. B) NDC field is incomplete. Entry does not contain a full
11 numbers, but is a combination of blanks and numbers. C) We have learned that some software packages are
converting your 11 digit NDC code entry to a five digit alpha/numeric code
for some over the counter items that used to be billed using the alpha/numeric
code but have now been assigned an 11 digit NDC code. D) Conversely, other software packages are converting
your 5 digit alpha/numeric HCPCS code entry to an 11 digit NDC code. These
items used to be billed using an NDC code but have been changed to a five
digit alpha/numeric code. Note: If
you receive a rejection code for your NDC entry, you should check with your
software vendor to see what code is being transmitted. E)
The Compound Code
field must contain a value of 1 for each NDC entry. An entry of any other
code in the compound code field when submitting an 11 digit NDC code will
cause a rejected claim. F)
The Product/Service Id
Qualifier (436-E1) field does not contain a value of 03. |
|
710 Maximum
Quantity Exceeded |
76 Plan
Limitations Exceeded |
0000100000 (100
Tablets) 0000001000 (1
package of gauze pads) 0000075000 (75
Caloric Units) |
1. The Quantity Dispensed is a 10 digit numeric field,
which contains 3 decimal positions. 2. The quantity that you enter in this field is checked
against the maximum quantity on the Drug Plan File for each drug or supply
item. If the amount entered exceeds the amount on the Drug Plan File, the
claim will deny. 3. If you have received prior approval to dispense a
quantity that exceeds the established maximum, you must enter the prior approval
number on your transaction. This will allow your claim to override the edit. 4. Some incorrect entries being received are: A)
00500 - The number of
items in a box or package are being submitted rather than the number of boxes
or packages. If there are 500 gauze pads in 1 box, the quantity should be
submitted as 0000001000. |
|
712 Override
Denied UT Not at Limit |
34 M/I
Prescription Denial Override |
00 (No
Override required) 01 (No
Override Required) 02 (UT
Service Authorization Exception Code P - Override Pending) 07 (UT
Service Authorization Exception Code J or L - Immediate Urgent Care or
Emergency) |
1. An entry must be placed in the Submission
Clarification Code field. 2. If the recipient is not at their UT limit, 00 or 01
should be entered. 3. If the recipient is at their limit, value 02 or 07
should be entered to override the limit. 4. Code 712 is returned if a value of 02 or 07 is
entered and the recipient has not reached their limit. |
|
999 Header Field Error |
None |
None – Please resubmit using NCPDP Version 5.1 |
Used for various Header errors, also used to indicate non-HIPAA complaince. |
|
320 Other Insurance Information Inconsistent |
85 Claim Not Processed |
COB Segment: Field 342-HC “99” (First
Occurrence) Field 431-DV = $100.00 |
1. Your claim will deny if the Medicare Deductible reported
on your claim is either greater than the Federal maximum deductible, or
non-numeric. Refer to the amount entered in field 431-DV, after the first
occurrence of qualifier “99” in field 342-HC on your claim in the COB
segment. The amount entered cannot be more than the Federal maximum
deductible, or non-numeric. |
|
COB Segment: Field 342-HC “07” Field 431-DV = $50.00 or
(Blank if no Medicare Involvement) |
2. If a claim is being denied for the Medicare
approved amount non-numeric, this would be caused by the dollar amount
entered in field 431-DV following qualifier “07” in field 342-HC, (Medicare
approved Amount) on your claim. The Medicare approved Amount must be either
blank, (if Medicare is not involved), or numeric (if Medicare is involved). |
||
|
320 Other Insurance Information Inconsistent |
85 Claim Not Processed |
COB Segment: Field 342-HC “08” Field 431-DV = $25.00 or
(Blank if no Medicare Involvement) |
3. Your claim will deny when the Medicare Paid amount
is non-numeric. The Medicare Paid amount must be blank (if Medicare is not
involved), or numeric (if Medicare is involved). |
|
320 Other Insurance Information Inconsistent |
85 Claim Not Processed |
COB Segment: Field 342-HC “07” Field 431-DV = $100.00 Field 342-HC “08” Field 431-DV = $80.00 Field 342-HC “99” Field 431-DV = $10.00
(Deductible Amount) Field 342-HC “99” Field 431-DV = $10.00
(Coinsurance Amount) Field 342-HC “99” Field 431-DV = $00.00
(Copay Amount) |
4. If the Medicare Data reported on the claim is
inconsistent, your claim will be denied. This denial will result when the
Medicare Approved Amount is completed and the Medicare paid amount is blank,
or the Medicare paid amount is completed and the Medicare Approved amount is
blank. Denial can also occur if the sum of the Deductible, Coinsurance and
Copay amount reported on the claim is greater than the difference between
the Medicare Approved amount and Paid Amounts. |
|
320 Other Insurance Information Inconsistent |
85 Claim Not Processed |
Pricing Segment: Field 426-DQ = $100.00
(Total Amount Charged) COB Segment: Field 342-HC “07” Field 431-DV = $80.00
(Medicare Approved Amount) |
5. When the Amount Charged that is reported on your
claim in field 426-DQ in the Pricing Segment, is less than the Medicare
Approved Amount reported on your claim, it will deny. |
|
320 Other Insurance
Information Inconsistent |
85 Claim Not Processed |
COB Segment: Field 342-HC “07” Field 431-DV = $150.00 Field 342-HC “08” Field 431-DV = $120.00 Field 342-HC “99” Field 431-DV = $00.00
(Deductible Amount) Field 342-HC “99” Field 431-DV = $30.00
(Coinsurance Amount) Field 342-HC “99” Field 431-DV = $00.00
(Copay Amount) |
6. Your Claim will deny when the Medicare Coinsurance
Amount Reported on the claim is non-numeric. When the second occurrence of
Identifier “99” is reported, and the Coinsurance Amount contains spaces,
blanks, or is alpha-numeric, the claim will be rejected. |
|
320 Other Insurance Information Inconsistent |
85 Claim Not Processed |
COB Segment: Field 342-HC “07” Field 431-DV = $125.00 Field 342-HC “08” Field 431-DV = $60.00 Field 342-HC “99” Field 431-DV = $50.00
(Deductible Amount) Field 342-HC “99” Field 431-DV = $15.00
(Coinsurance Amount) Field 342-HC “99” Field 431-DV = $00.00
(Copay Amount) |
7. Your Claim will deny when the Medicare Copayment
Amount Reported on the claim is non- numeric. When the third occurrence of
Identifier “99” is reported, and the Copay Amount contains spaces, blanks,
or is alpha-numeric, the claim will be rejected. |
|
306 Item Requires Manual Review |
85 Claim Not Processed |
COB Segment: Field 342-HC “07” Field 431-DV = $100.00 Field 342-HC “08” Field 431-DV = $80.00 |
1. When the Medicare Paid Amount Reported on the claim
is less than reasonable, your claim will pend. The system will allow up to
the Federal maximum for the deductible, and a maximum of 20% Coinsurance
payment. If the amounts entered on the claim do not conform to the logic,
your claim will pend. |
|
717 Client
has Other Insurance |
85 Claim Not
Processed |
COB Segment: Field 342-HC “08” Field 431-DV = $75.00
(Medicare Paid Amount) |
1. If the Medicaid Client has Medicare Part B Outpatient coverage on file, and the NDC/HCPCS code being billed is flagged as payable by Medicare, and the Medicare paid amount reported on the claim is spaces or non-numerics, your claim will deny. |
|
Code |
Description |
|
127 |
Co-payment
Requirements Have Been Met |
|
128 |
No Co-payment Required
– Recipient Under 21 or Exempt |
All of the Table 7 codes are denial codes. Their presence in your response means that the claim has been rejected. If none of the Table 7 codes apply to your claim, you will see 000 in your response instead.
|
MEVS CODE |
DESCRIPTION |
NCPDP CODE |
DESCRIPTION |
|
132 |
M/I Item / NDC Code |
21 |
M/I Product/Service Id |
|
133 |
Product/Service Not
Covered for Patient Gender |
61 |
Drug Not Covered for
Patient Gender |
|
134 |
Patient Age Exceeds
Maximum Age |
66 |
Patient Age Exceeds
Maximum Age |
|
135 |
Patient Age Precedes
Minimum Age |
85 |
Claim Not Processed |
|
136 |
Requested Item Exceeds
Frequency Limitation |
85 |
Claim Not Processed |
|
137 |
Missing/Invalid
Quantity Dispensed |
E7 |
M/I Quantity Dispensed |
|
140 |
Category of service not
valid for item / NDC code |
05 |
M/I Pharmacy Number |
|
142 |
Missing / Invalid
category of service |
05 |
M/I Pharmacy Number |
|
705 |
NDC/APC Not Covered |
70, 77 |
Product/Service Not
Covered, Discontinued Product/Service Id Number |
|
706 |
Refill Code Exceeds
Number of Refills Authorized |
17 |
M/I Fill Number |
|
707 |
Previously Filled
Refill |
17 |
M/I Fill Number |
|
708 |
Exceeds NY Allowed
Refill Maximum |
29 |
M/I Number Refills
Authorized |
|
709 |
Maximum Day’s Supply Exceeded |
19 |
M/I Days Supply |
|
710 |
Maximum Quantity
Exceeded |
76 |
Plan Limitations
Exceeded |
|
711 |
Date Filled Prior to
Date Rx Written |
28 |
M/I Date Prescription
Written |
|
712 |
Override Denied - UT
not at limit |
34 |
M/I Submission
Clarification Code |
|
713 |
Refill over 180 days
from Date Rx Written |
28 |
M/I Date Prescription
Written |
|
714 |
Date Filled More than
60 days from Date Rx Written |
28 |
M/I Date Prescription
Written |
|
715 |
Other Insurance Amount
must be greater than zero |
13 |
M/I Other Coverage Code |
|
716 |
Other Insurance Amount
must be equal to zero |
13 |
M/I Other Coverage Code |
|
717 |
Recipient has Other
Insurance |
13 |
M/I Other Coverage Code |
|
718 |
HR Recipient - No
Rebate Agreement |
77 |
Discontinued
Product/Service Id Number |
|
719 |
MA Only Covers Family
Planning |
65 |
Patient Is Not Covered |
|
720 |
Days Supply is Less
than the Minimum Required |
19 |
M/I Days Supply |
|
722 |
Family Health Plus
Denial |
65 |
Patient is Not Covered |
The chart starting on the following page lists the most frequently returned reject denial codes from Table 7 and describes the entry errors being received.
|
CODE |
DESCRIPTION |
APPROVAL OR DENIAL |
PROCESSING RESULTS DESCRIPTION |
|
AA |
UT Approved, P&C
Approved |
A |
UT&P&C S/A |
|
AD |
UT Approved, Services
Not Ordered |
D |
No S/A |
|
AN |
UT Approved, P&C
Not Invoked |
A |
UT S/A |
|
DA |
UT At Service Limits,
P&C Approved |
D |
No S/A |
|
DD |
UT At Service Limits,
Services Not Ordered |
D |
No S/A |
|
DN |
UT At Service Limits,
P&C Not Invoked |
D |
No S/A |
|
LA |
UT Approved Near
Limits, P&C Approved |
A |
UT&P&C S/A |
|
LD |
UT Approved Near
Limits, Services Not Ordered |
D |
No S/A |
|
LN |
UT Approved Near
Limits, P&C Not Invoked |
A |
UT S/A |
|
NA |
UT Not Invoked, P&C
Approved |
A |
P&C S/A |
|
ND |
UT Not Invoked,
Services Not Ordered |
D |
No S/A |
|
NN |
UT Not Invoked, P&C
Not Invoked |
A |
Exempt - No S/A
Necessary |
|
PA |
UT Override Denied,
P&C Approved |
D |
No S/A |
|
PD |
UT Override Denied,
Services Not Ordered |
D |
No S/A |
|
PN |
UT Override Denied,
P&C Not Invoked |
D |
No S/A |
|
XX |
DUR Denial |
D |
No S/A |
Table 8 codes were formulated to return a code which combines the Utilization Threshold (UT) and Post and Clear (P&C) programs. The first alpha character indicates the UT status; the second character indicates the P&C status. Both characters must indicate an approval in order for service authorizations to be generated. The key to recognizing an approval code:
The first character must be an "A", "L", or "N” and
The second character must be an "A" or "N".
The only Table 8 codes that indicate an approval for a UT and/or P&C service authorization are:
AA (UT and P&C service authorization)
AN (UT only, P&C exempt)
LA (UT and P&C service authorization)
LN (UT only - P&C exempt)
NA (UT exempt, P&C service authorization)
NN (UT exempt, P&C exempt)
Note: Although these are approval codes, the approval is for the UT and P&C programs only. The claim must pass all other editing in order for the authorizations to be considered approved for payment. If the response status field contains a "C" (Claim Captured), any necessary service authorizations have been established. If the response status field contains an "R" (Rejected), no authorizations are generated. A Table 8 code is returned in every response even if the claim is rejected.
The third column in Table 8 lists the approval (A) or denial (D) status of each code.
The fourth column in Table 8 indicates whether service authorization requirements were satisfied.
Not invoked means that the claim did not have to be processed through that designated program. For example: UT Not Invoked means that the claim was not processed through the UT program for various reasons. (Recipient may be exempt from UT, etc).
If the claim is denied for DUR (Code XX), the UT and P&C status code will not be displayed because the UT, P&C approval has been negated by the DUR denial.
|
CODE |
DESCRIPTION |
|
129 |
Duplicate/Redundant DVS
request |
|
130 |
DVS process was not invoked |
|
131 |
Item approved / DVS number
issued |
|
132 |
Missing / Invalid item /
NDC code |
|
133 |
Item not covered for
patient gender |
|
134 |
Patient age exceeds maximum
age |
|
135 |
Patient age precedes
minimum age |
|
136 |
Requested item exceeds
frequency limitation |
|
137 |
Missing / Invalid quantity
dispensed |
|
139 |
DVS requires current date
entry |
|
140 |
Category of service not
valid for item / NDC code |
|
142 |
Missing / Invalid category of service |
|
705 |
NDC/HCPCS Not Covered |
|
710 |
Maximum Order Quantity
Exceeded |
|
CODE |
DESCRIPTION |
|
301 |
Pending for Manual
Pricing. (The NDC being billed requires manual review and pricing by DOH). |
|
306 |
Item Requires Manual
Review. (The NDC being billed requires manual review by DOH prior to
payment). |
|
310 |
Pharmacy Service
Included in In-state Facility Rate |
|
311 |
PCP Plan Code Not on
Contract File. (Recipient is enrolled in a managed care plan but the plan
code has not yet been added to DOH’s Managed Care Contract file). Call
Provider Services 1-800-343-9000 |
|
317 |
Claim Pending: Excess
Income/Spenddown. (Recipient has income in excess of the allowable Medicaid
levels and will be considered eligible for Medicaid reimbursable services
only at the point his/her excess income is reduced to the appropriate level.
This response will be issued if you override the excess income denial [code
104] and the LDSS has not yet updated eligibility on the Client database). |
|
319 |
Prior Approval Not on
or Removed From File. (PA is not found on or no longer active on the eMedNY
contractor’s PA file). |
Note: These codes may appear in the Table 2 response area for non-ECCA transactions since non-ECCA transactions will not be held in a pending status. They will be rejected if the conditions for these reason codes exist.
|
CODE |
DESCRIPTION - M/I =
Missing/Invalid |
MEVS CODE |
|
01 |
M/I BIN |
|
|
04 |
M/I Processor Control
Number |
702,703, 704 |
|
05 |
M/I Pharmacy Number |
051, 092, 140, 142 |
|
07 |
M/I Cardholder ID
Number |
030, 031, 033, 061, 062 |
|
08 |
M/I Person Code |
063 |
|
09 |
M/I Birthdate |
300, 700 |
|
10 |
M/I Patient Gender Code |
701 |
|
13 |
M/I Other Coverage Code |
715, 716, 717 |
|
14 |
M/I Eligibility
Clarification Code |
|
|
15 |
M/I Date of Service |
071 |
|
16 |
M/I
Prescription/Service Reference Number |
|
|
17 |
M/I Fill Number Code |
706, 707 |
|
19 |
M/I Days Supply |
709, 720 |
|
20 |
M/I Compound Code |
|
|
21 |
M/I Product/Service Id |
132 |
|
22 |
M/I Dispense as Written
Code (DAW) Product Selection Code |
|
|
25 |
M/I Prescriber ID |
056, 059, 066, 067, 068, 318 |
|
28 |
M/I Date Prescription
Written |
711, 713, 714 |
|
29 |
M/I Number Refills
Authorized |
708 |
|
34 |
M/I Submission
Clarification Code |
712 |
|
35 |
M/I Primary Care
Provider Id |
100, 101, 118 |
|
50 |
Non-Matched Pharmacy
Number |
052 |
|
52 |
Non-Matched Cardholder
ID |
065 |
|
61 |
Product/Service Not
Covered For Patient Gender |
133 |
|
65 |
Patient is Not Covered |
001, 103, 104, 719, 722 |
|
66 |
Patient Age Exceeds
Maximum Age |
134 |
|
70 |
Product/Service Not
Covered |
705 |
|
75 |
Prior Authorization
Required |
|
|
76 |
Plan Limitations
Exceeded |
710 |
|
77 |
Discontinued
Product/Service Id Number |
705, 718 |
|
81 |
Claim Too Old |
702 |
|
82 |
Claim is Post Dated |
|
|
83 |
Duplicate Paid/Captured
Claim |
|
|
84 |
Claim Has Not Been
Paid/Captured |
|
|
85 |
Claim Not Processed |
|
|
87 |
Reversal Not Processed |
045 |
|
88 |
DUR Reject Error |
|
|
92 |
System Unavailable |
324 |
|
DQ |
M/I Usual and Customary |
|
|
DV |
M/I Other Payor Amount
Paid |
320 |
|
DX |
M/I Patient Paid Amount
Submitted |
|
|
EV |
M/I Prior Authorization
Number Submitted |
303, 304, 319 |
|
E1 |
M/I Product/Service Id
Qualifier |
|
|
E4 |
M/I Reason for Service
Code |
|
|
E6 |
M/I Result for Service
Code |
|
|
E7 |
M/I Quantity Dispensed |
137 |
|
MZ |
Error Overflow |
|
Up to twenty (20) NCPDP reject codes can appear in the rejected response. If a code has a comparable MEVS reject code that code will also be returned in the response. Most of the NCPDP reject codes are self-explanatory or have been further explained in other sections. Those needing further clarification are described below.
Code 22 - M/I Dispense As Written Code:
An entry is required. The acceptable values are:
0 - No Product Selection Indicated.
1 - Substitution not allowed by Prescriber.
4 - Substitution allowed - Generic Drug not in stock.
5 - Substitution allowed - Brand Drug Dispensed as a Generic.
7 - Substitution not allowed - Brand Drug mandated by law.
8 - Substitution allowed - Generic Drug not available in marketplace.
Code EV - M/I Prior Authorization Number Submitted
Code:
If an NDC or HCPCS requires a prior approval number, the prior approval field must contain the prior approval number assigned to you for the NDC or HCPCS. The prior approval field is 11 digits in length. The first 8 digits should contain the prior approval number followed by three zeroes. Example 56734268000. Additionally, the Prior Authorization Type Code (461-EU) field should contain a “01” if reporting a PA number with no co-pay exemption. If the patient is co-pay exemption, enter a number “04”.
Code 83 - Duplicate Paid/Captured Claim:
This code is returned when a claim is submitted and the Service Product Id Number, Cardholder ID, Date of Service, and Prior Authorization Number Submitted fields match a previously paid claim and one of the following three conditions also exist:
· Prescription/Service Reference Number, NDC/HCPCS (if not a compound), and Generic Code match, but the Fill Number Code is different.
· Prescription/Service Reference Number and Generic Code match, but NDC/HCPCS is different
· NDC/HCPCS (if not a compound) match, but Prescription/Service Reference Number is different.
Refer to section 2.14 on page 2.14.1 for additional information.
Code 84 - Claim Has Not Been Paid/Captured:
This code is returned when a transaction is submitted (transactions codes N1 and N3) with the intent of supplying DUR information only for purposes of updating the recipient's drug history file when no claim submission or reimbursement is allowed or expected. If Code 84 is the only code returned, the drug history file has been updated.
DQ - M/I Usual and Customary:
An entry is required in the Usual and Customary Charge field. If the claim is being sent for ECCA processing, the amount in this field must be greater than zeroes. If ECCA is not being requested, the field must be zero filled.
Several abbreviations are used when referring to the Drug Utilization Program. These abbreviations are listed below with a brief description.
|
|
|
|
CPU |
Central Processing Unit. This is also known as the mainframe computer. |
|
CPU-CPU Link |
A direct telecommunication connection to the eMedNY contractor’s mainframe computer using a central processing unit to access the MEVS/Pro-DUR systems. |
|
DME |
Durable Medical Equipment. These items and their codes are listed in the DME MMIS Provider Manual and are further identified by use of specialty code 307 or category of service 0442 when billing and must be submitted on a DME claim form. Some DME item codes require a DVS number. These must be submitted by using a 278 ASC X12N transaction, the Verifone Omni 3750 Terminal or ePACES. |
|
DVS |
Dispensing Validation System. This feature allows you to obtain the required prior approval number (DVS number) for pre-designated DME item codes and certain prescription drugs in the same transaction as your DUR/ECCA claim. Items, which are only reimbursable under COS 0442, cannot be submitted through the NCPDP format. |
ECCA |
Electronic Claims Capture and Adjudication. This is an optional feature of the Pro-DUR program, which allows you to have your DUR claim captured and adjudicated for payment by the eMedNY contractor. |
ETIN |
Electronic Transmitter Identification Number. A three-character code assigned by the eMedNY contractor to a provider who wishes to send their claims electronically or via magnetic media. The Electronic Transmitter Identification Number has also been referred to as a Magnetic Supplier Number. Each pharmacy must submit their ETIN with a notarized certification statement to the eMedNY contractor. The ETIN must be entered on each Pro-DUR transaction in order to have the claim electronically captured. |
|
HCPCS |
Health Care Financing Administration Common Procedure Coding System. The five digit alpha/numeric HCPCS code is assigned by CMS to over the counter sickroom supplies. These codes are found in sections 4.2 and 4.3 in the MMIS Pharmacy Provider Manual. The five digit alpha/numeric DME item codes are also entered as HCPCS codes for DVS Transactions. |
|
MEVS |
Medicaid Eligibility Verification System. The system which processes providers’ eligibility inquiries and service authorization requests for New York State Medicaid recipients. |
|
LICENSE TYPE |
Two digit code indicating the type of provider that wrote the prescription. The valid license types are: 01 NYS Physician 02 NYS Dentist 09 NYS Physician Assistant 25 NYS Optometrist 26 NYS Podiatrist 27 NYS Audiologist 29 NYS Nurse Practitioner/Midwife 11 Out-of-State Physician 12 Out-of-State Dentist 19 Out-of-State Physician Assistant 35 Out of State Optometrist 36 Out-of-State Podiatrist 37 Out-of-State Audiologist 39 Out-of-State Nurse Practitioner/Midwife |
|
MAGNETIC MEDIA |
Tape, Cartridge, or Diskette used to submit claims for processing. |
|
NCPDP |
National Council for Prescription Drug Program. A nonprofit membership organization working toward the standardization and efficiency of third party prescription drug program processing. New York State is using NCPDP's Version 5.1 Telecommunication Standard and the 1.1 Batch formats to administer the DUR program and have your DUR claim captured and adjudicated for payment by the eMedNY contractor. |
|
NDC |
National Drug Code. The eleven digit number assigned to each drug or OTC item. |
|
NYSDOH |
New York State Department of Health |
|
OTC |
Over the Counter drug or supply which does not require a prescription. |
|
P & C |
Post and Clear. The program in effect which requires certain prescribers to post their prescriptions on the MEVS system. The posted prescriptions must then be "cleared" by the dispensing provider. P&C service authorizations are required for payment to be made. |
|
PC |
Personal Computer. |
|
PC-Host Link |
A Dial-Up into the MEVS network using a personal computer to access the MEVS/Pro-DUR systems. |
|
PIN |
Personal Identification Number. A four digit number selected by each pharmacy and submitted to the New York State Department of Health for input to the pharmacy's provider file. Pharmacies must enter the number on each Pro-DUR transaction in order to have their claim electronically captured and submitted for adjudication. |
|
Pro-DUR |
Prospective Drug Utilization Review. This is a mandatory program, which alerts pharmacists to possible contraindications when dispensing drugs to a recipient. |
|
Switch (Switching) |
A company that passes the Pro-DUR/ECCA transaction from the provider to the MEVS network, via a dedicated telecommunications link, and returns the response from the MEVS network to the provider. |
|
TSN |
Transmission Supplier Number. Refer to Electronic Transmitter Identification Number (ETIN). |
|
UT |
Utilization Threshold. The mandatory program in effect, which limits Medicaid recipients to a designated number of services, prescriptions, etc. per year. Providers must receive a UT service authorization in order for payment to be made. |
A: If you have any questions regarding your software, refer them to your software vendor. The New York State Department of Health and the eMedNY contractor do not have any control over software written to interface with the Pro-DUR/ECCA system.
Q: What phone number do I dial to access the production Pro-DUR/ECCA system?
A: For PC-Host going direct to the eMedNY contractor, you will receive the production phone numbers once you have completed certification and testing.
For providers going through a switch, you should contact your switch for access procedures and information.
Q: What is my PIN?
A: The Provider Services Department staff can verify if the PIN you are using is correct. They are not authorized to give out your PIN number for security reasons. If you do not know your PIN number, you must complete a new "PIN Selection Form" and return it to New York State Department of Health.
Q: What is my ETIN?
A: Contact Provider Services at 1-800-343-9000 for the ETIN that is authorized for electronic processing.
Q: Will my claim be paid?
A: If your claim is electronically captured and approved for payment, your claim will be paid. One exception to this rule is for excess income/spenddown. Once you have overridden the 104 denial response, your claim will pend waiting for an eligibility update from the WMS. If the update is not timely, your claim will release from its pending status and deny. These “captured, then denied” claims will appear on your remittance statement as being denied. Refer to the Electronic Claims Capture and Adjudication section on page 2.4.1 of the manual for additional information.
Q: Why am I getting "NO CLAIM TO FA"?
A: You receive this message any time the system has determined the claim can not be captured for adjudication. There are many reasons for this, including if the Processor Control Number is not submitted. Refer to the Electronic Claims Capture and Adjudication section on page 2.4.1 of the manual for additional information.
Q: Will this claim be paid online?
A: Your claim will be fully adjudicated. Claims approved for payment will appear as paid within the remittance statement issued for that payment cycle.
Q: What is Person Code?
A: The Person Code is the NCPDP field used to input the Recipient's Sequence Number. The sequence number can be found on the recipient's card.
Q: I received a DUR warning for high dosage and refills too early and my claim was denied? Why?
A: In the online Pro-DUR/ECCA system, the eMedNY contractor sends back warning information about certain drug interactions. These are only warnings and are NOT rejects in the online system. Some software companies will treat these warnings as REJECTS when interpreting the DUR response. You need to talk to your software provider to determine how to deal with this condition.
Q: What is the valid NDC code for a particular drug?
A You should look at the microfiche you receive from New York Medicaid. All reimbursable drugs are listed. If you cannot find it, you can call New York State Department of Health at 1-518-486-3209.
Q: What is the proper procedure for entering sickroom supplies using Health Care Financing Administration Common Procedure Coding System (HCPCS)?
A: Refer to Section 2.8 (page 2.8.1) on HCPCS Codes in the manual for clarification.
Q: Was a UT service authorization produced by the eMedNY contractor?
A: Refer to Table 8 (page 13.0.1) on UT, P&C codes in this manual for clarification.
Q: Why am I getting M/I Prior Authorization Number Submitted? This doesn't need a PA!
A: If the item you are entering does not need Prior Approval/Authorization and you're using the version 5.1 format, the Prior Auth Number Submitted (462-EV) field should not be transmitted (your software system should take care of this).
Q: How should the Prior Auth Type Code 461-EU and Prior Auth Number Submitted 462-EV be put in the field?
A: The first field (461-EU) should contain a ‘01’ for Prior Auth Number submission or ‘04’ to identify co-pay exempt. If a P.A. No. is also required with the co-pay exempt then submit as follows: The second field (462-EV), positions 1 thru 8 = prior approval number and positions 9 thru 11 = zeroes (000) when 461-EU contains ‘01’. If 461-EU contains ‘04’ for co-pay exempt and does not require a P.A. No., do not submit 462-EV. If a P.A. No. is also required then submit 462-EV as indicated above.
Refer to Section 2.11 on page 2.11.1 for field descriptions.
Q: Why was I rejected?
A: Refer to Table 2 (page 10.0.1), Table 7 (page 12.0.1), Table 8 (page 13.0.1), Table 9 (page 14.0.1) and the NCPDP Reject Codes list for clarification.
Q: What were my DUR reject codes, I cleared my screen already?
A: You should first check with your software vendor to see if there is a method of recovering or re-displaying the response for a transaction. If there is not, you can resubmit the transaction and get the same errors.
Q: I received DUR Reject Code 85 in my response, what does it mean?
A: You should look for the accompanying error codes that are part of the response in the Additional Message field. The first is the MEVS Accepted or Denial code. This code is in the first three positions. The other code is the Rx Denial Code. It follows the MEVS code and a space. Additionally, the claim could be rejected because of UT/P&C denials or DVS denials. Refer to Table 2 (page 10.0.1), Table 7 (page 12.0.1), Table 8 (page 13.0.1), Table 9 (page 14.0.1) in this manual.
Q: Why does it say M/I Product/Service ID or Product/Service Not Covered, when the NDC is in fact covered?
A: Refer to Table 7 (page 12.0.1) error chart for further explanation.
Q: What is Maximum Quantity, or Plan Limitations exceeded?
A: The maximum quantity or plan limitations reject is when the amount in the Quantity Dispensed field is greater than the allowed or approved New York State Medicaid quantity. For assistance call Provider Services at 1-800-343-9000.
Q: I am getting a reject code of 100 or 101, what do I do?
A: Refer to Table 2 (page 10.0.1) error chart for further explanation.
Q: What is E4 Reason for Service Code or E6?
A: These are both NCPDP Reject Codes. The E4 code indicates there is a problem with the Reason for Service Code input with the claim. It could be because the data is not one of the DUR reject conflict codes, a DUR override was not required, or the field was the wrong size. The E6 code indicates there is a problem with the Result for Service Code. The common problems are a DUR override is not needed or the wrong value was input. Another common problem is only one of the fields is entered. Both fields should be reviewed and the transaction resubmitted. Refer to the Override Processing section for further clarification.
Q: How do I process an override?
A: There are four types of overrides for transactions. The first is the MEVS UT or Utilization Threshold override. It is entered in NCPDP Submission Clarification Code (420-DK) field. The UT override is needed when you receive a UT Denial or a D in the first position of the codes for UT/PC in Additional Message (526-FQ) field. The second override is for DUR. This is entered in Reason for Service Code (439-E4) field. The DUR override is required when you receive a DUR Reject, error code 88. Both can be entered in the same transaction. Beware; if the override is not required, the transaction will be rejected. Refer to the Override Processing section for further clarification. The third override is the excess income/spenddown override. This override can be entered in the Eligibility Clarification Code (309-C9) field to override response code 104. Once overridden, your claim will be captured if the processor control number field is completed properly. Once captured, your claims will pend, waiting for a WMS eligibility update to occur. If the update is not timely, your claim will appear as denied on your remittance statement.
The fourth override is the Nursing Home override. The Eligibility Clarification Code (309-C9) field may also be used to report a Nursing Home Override. You may use this override code when resubmitting a previously denied claim if a Client is a resident of an In-State Skilled Nursing Facility which includes coverage for pharmacy services. This will result in a pend status which will allow local districts time to update the Client’s file if the patient has been discharged from the Facility.
The following forms are included in the manual:
Personal Identification Number Request
Certification Statement For Provider Utilizing Electronic Billing
|
Provider
Number |
|
|
||||||||||||||
|
Provider
Name |
|
|
||||||||||||||
|
Provider
Address |
|
|
||||||||||||||
|
|
|
|
||||||||||||||
|
|
|
|
||||||||||||||
|
|
|
|
||||||||||||||
|
Pin Number |
|
|
|
|
|
|
|
|
|
|||||||
|
|
(Any four (4) digits) |
|||||||||||||||
|
Name |
|
|
||||||||||||||
|
(Print of Type) |
|
|||||||||||||||
|
Signature |
|
Date |
|
|||||||||||||
|
|
|
|
||||||||||||||
|
Telephone
Number |
( ) |
|
||||||||||||||
|
Return To: New York State Department of Health Suite 608 99 Washington Avenue Albany, NY 12210 Attn: Diane Sumell |
||||||||||||||||
ETIN (1) BILLING SERVICE NAME (IF
APPLICABLE (2)
MEDICAID MANAGEMENT INFORMATION SYSTEM
As of (date) (3) and for one year after this date all claims
electronically submitted to the State's Medicaid fiscal agent, for services or
supplies furnished by (provider name) (4) (provider
number) (5) will be subject to the following
certification.
I am (or the business entity
named on this form of which I am a partner, officer or director is) a qualified
provider enrolled with and authorized to participate in the New York State
Medical Assistance Program and in the profession or specialties, if any,
required in connection with this claim; the person(s) providing services, care
or supplies have the required licensing, certification and training. I have reviewed this form; I (or the entity)
have furnished or caused to be furnished the care, services and supplies
itemized and I or the entity make this claim in accordance with applicable
federal and state laws and regulations.
I certify that the services were rendered at the location listed in the
“place of service field” and that such location has been entered on the
claim. I HAVE READ THE MEDICAID
MANAGEMENT INFORMATION SYSTEMS PROVIDER MANUAL AS IT RELATES TO THE CLAIM FORM,
AND ALL REVISIONS AND UPDATES THERETO; ALL CLAIMS ARE MADE IN FULL COMPLIANCE
WITH THE PERTINENT PROVISIONS OF THE MANUAL, REVISIONS AND UPDATES; ALL CLAIMS
FOR CARE SERVICES AND SUPPLIES PROVIDED AT THE ORDER OF ANOTHER PROFESSIONAL
HAVE TO THE BEST OF MY KNOWLEDGE BEEN ORDERED BY THAT PROFESSIONAL IN BONA FIDE
COMPLIANCE WITH THE PROCEDURES SET FORTH IN THE MANUAL, REVISIONS, OR UPDATES
AND ALL FEDERAL AND STATE LAWS AND REGULATIONS. ALL CARE, SERVICES, AND SUPPLIES FOR WHICH CLAIM IS MADE ARE
MEDICALLY NECESSARY FOR THE TREATMENT OF THE NAMED RECIPIENT. The amounts listed are due and, except as
noted, no part thereof has been paid by, or to the best of my knowledge is
payable from any source other than, the Medical Assistance Program; payment of
fees made in accordance with established schedules is accepted as payment in
full; other than a claim rejected or denied or one for adjustment, no previous
claim for the care, services and supplies itemized has been submitted or paid;
ALL. STATEMENTS MADE HEREON ARE TRUE, ACCURATE AND COMPLETE TO THE BEST OF MY
KNOWLEDGE; NO MATERIAL FACT HAS BEEN OMITTED FROM THIS FORM; I UNDERSTAND THAT
PAYMENT AND SATISFACTION OF THIS CLAIM WILL BE FROM FEDERAL, STATE AND LOCAL
PUBLIC FUNDS AND THAT I MAY BE PROSECUTED UNDER APPLICABLE FEDERAL AND STATE
LAWS FOR ANY FALSE CLAIMS, STATEMENTS OR DOCUMENTS OR CONCEALMENT OF A MATERIAL
FACT; taxes from which the State is exempt are excluded; all records pertaining
to the care, services and supplies provided including all records which are
necessary to disclose fully the extent of care, services and supplies provided
to individuals under the New York State Medical Assistance Program will be kept
for a period of six years from the date of payment, and such records and
information regarding this claim and payment therefor shall be promptly
furnished upon request to the local social services district or the New York
State Department of Health, the State Medicaid Fraud Control Unit or the
Secretary of the Department of Health and Human Services; there has been
compliance with the Federal Civil Rights Act of 1964 and with section 504 of
the Federal Rehabilitation Act of 1973, as amended, which forbid discrimination
on the basis of race, color, national origin, handicap, age, sex and religion;
I agree (or the entity agrees) to comply with the requirements of 42 CFR Part
455 relating to disclosures by providers; the State of New York through its
fiscal agent or otherwise is hereby authorized to (1) make administrative
corrections to this claim to enable its automated processing subject to
reversal by provider, and (2) accept the claim data on this form as original
evidence of care, services and supplies furnished.
By making this claim I
understand and agree that I (or the entity) shall be subject to and bound by
all laws, rules, regulations, policies, standards, fee codes and procedures of
the United States Department of Health and Human Services, the New York State
Department of Health (Department) and other publications of the Department,
including Medicaid Management Information System Provider Manuals and other
official bulletins of the Department or any other law, rule, regulation,
policy, procedures of any other state agency which governs the provision of or
billing for care, services or supplies which are reimbursed under the Medical
Assistance Program for the State of New York. I understand and agree that I (or
the entity) shall be subject to and shall accept, subject to due process of
law, any determinations pursuant to said rules, regulations, policies,
standards, fee codes and procedures, including, but not limited to, any duly
made determination affecting my (or the entity’s) past, present or future
status in the Medicaid program and/or imposing any duly considered sanction or
penalty. I further certify that I have
complied with the billing requirements of the United States Department of
Health and Human Services and the Department including but not limited to the
following: If I am billing as an
individual provider (individual practitioner or business entity which is not
required to enroll as a group), I certify that the care, services or supplies
were provided by me except in situations where care, services or supplies were
provided: (a) under a locum tenens
agreement or (b) by a physician’s assistant or certified social worker who was
under my supervision, and that my provider identification number is being used
on the claim for payment. If I am
required to bill as a group provider, I certify that the care, services or
supplies were provided by the group, that the provider identification number of
the group is being used on the claim for payment, and that the provider
identification number of the individual who provided the service has been
entered on the claim.
I UNDERSTAND THAT MY
SIGNATURE HEREON GUARANTEES THE ABOVE CERTIFICATION WILL APPLY TO ALL
ELECTRONIC CLAIMS SUBMITTED, USING MY (OR THE ENTITY'S) MEDICAID PROVIDER
IDENTIFICATION NUMBER.
(Signature) (6)
(Date) (7)
(Typed Name and Title) (8)
STATE OF NEW YORK
COUNTY OF (9)
On this day of , 20
,before me personally came , to me known and known to me to be the
individual described in and who executed the foregoing instrument, and (s)he
acknowledged to me that (s)he executed the same.
(SEAL)
NOTARY
PUBLIC
ETIN BILLING
SERVICE NAME (IF APPLICABLE
MEDICAID MANAGEMENT INFORMATION SYSTEM
As of (date) and for one year
after this date all claims electronically submitted to the State's Medicaid
fiscal agent, for services or supplies furnished by (provider name) (provider
number)
will be subject to the following certification.
I am (or the business entity
named on this form of which I am a partner, officer or director is) a qualified
provider enrolled with and authorized to participate in the New York State
Medical Assistance Program and in the profession or specialties, if any,
required in connection with this claim; the person(s) providing services, care
or supplies have the required licensing, certification and training. I have reviewed this form; I (or the entity)
have furnished or caused to be furnished the care, services and supplies
itemized and I or the entity make this claim in accordance with applicable
federal and state laws and regulations.
I certify that the services were rendered at the location listed in the
“place of service field” and that such location has been entered on the
claim. I HAVE READ THE MEDICAID
MANAGEMENT INFORMATION SYSTEMS PROVIDER MANUAL AS IT RELATES TO THE CLAIM FORM,
AND ALL REVISIONS AND UPDATES THERETO; ALL CLAIMS ARE MADE IN FULL COMPLIANCE
WITH THE PERTINENT PROVISIONS OF THE MANUAL, REVISIONS AND UPDATES; ALL CLAIMS
FOR CARE SERVICES AND SUPPLIES PROVIDED AT THE ORDER OF ANOTHER PROFESSIONAL
HAVE TO THE BEST OF MY KNOWLEDGE BEEN ORDERED BY THAT PROFESSIONAL IN BONA FIDE
COMPLIANCE WITH THE PROCEDURES SET FORTH IN THE MANUAL, REVISIONS, OR UPDATES
AND ALL FEDERAL AND STATE LAWS AND REGULATIONS. ALL CARE, SERVICES, AND SUPPLIES FOR WHICH CLAIM IS MADE ARE
MEDICALLY NECESSARY FOR THE TREATMENT OF THE NAMED RECIPIENT. The amounts listed are due and, except as
noted, no part thereof has been paid by, or to the best of my knowledge is
payable from any source other than, the Medical Assistance Program; payment of
fees made in accordance with established schedules is accepted as payment in
full; other than a claim rejected or denied or one for adjustment, no previous
claim for the care, services and supplies itemized has been submitted or paid;
ALL. STATEMENTS MADE HEREON ARE TRUE, ACCURATE AND COMPLETE TO THE BEST OF MY
KNOWLEDGE; NO MATERIAL FACT HAS BEEN OMITTED FROM THIS FORM; I UNDERSTAND THAT
PAYMENT AND SATISFACTION OF THIS CLAIM WILL BE FROM FEDERAL, STATE AND LOCAL
PUBLIC FUNDS AND THAT I MAY BE PROSECUTED UNDER APPLICABLE FEDERAL AND STATE
LAWS FOR ANY FALSE CLAIMS, STATEMENTS OR DOCUMENTS OR CONCEALMENT OF A MATERIAL
FACT; taxes from which the State is exempt are excluded; all records pertaining
to the care, services and supplies provided including all records which are
necessary to disclose fully the extent of care, services and supplies provided
to individuals under the New York State Medical Assistance Program will be kept
for a period of six years from the date of payment, and such records and
information regarding this claim and payment therefor shall be promptly
furnished upon request to the local social services district or the New York
State Department of Health, the State Medicaid Fraud Control Unit or the
Secretary of the Department of Health and Human Services; there has been
compliance with the Federal Civil Rights Act of 1964 and with section 504 of
the Federal Rehabilitation Act of 1973, as amended, which forbid discrimination
on the basis of race, color, national origin, handicap, age, sex and religion;
I agree (or the entity agrees) to comply with the requirements of 42 CFR Part
455 relating to disclosures by providers; the State of New York through its
fiscal agent or otherwise is hereby authorized to (1) make administrative
corrections to this claim to enable its automated processing subject to
reversal by provider, and (2) accept the claim data on this form as original
evidence of care, services and supplies furnished.
By making this claim I
understand and agree that I (or the entity) shall be subject to and bound by
all laws, rules, regulations, policies, standards, fee codes and procedures of
the United States Department of Health and Human Services, the New York State
Department of Health (Department) and other publications of the Department,
including Medicaid Management Information System Provider Manuals and other
official bulletins of the Department or any other law, rule, regulation,
policy, procedures of any other state agency which governs the provision of or
billing for care, services or supplies which are reimbursed under the Medical
Assistance Program for the State of New York. I understand and agree that I (or
the entity) shall be subject to and shall accept, subject to due process of
law, any determinations pursuant to said rules, regulations, policies,
standards, fee codes and procedures, including, but not limited to, any duly
made determination affecting my (or the entity’s) past, present or future
status in the Medicaid program and/or imposing any duly considered sanction or
penalty. I further certify that I have
complied with the billing requirements of the United States Department of
Health and Human Services and the Department including but not limited to the
following: If I am billing as an
individual provider (individual practitioner or business entity which is not
required to enroll as a group), I certify that the care, services or supplies
were provided by me except in situations where care, services or supplies were
provided: (a) under a locum tenens
agreement or (b) by a physician’s assistant or certified social worker who was
under my supervision, and that my provider identification number is being used
on the claim for payment. If I am
required to bill as a group provider, I certify that the care, services or
supplies were provided by the group, that the provider identification number of
the group is being used on the claim for payment, and that the provider
identification number of the individual who provided the service has been
entered on the claim.
I UNDERSTAND THAT MY
SIGNATURE HEREON GUARANTEES THE ABOVE CERTIFICATION WILL APPLY TO ALL
ELECTRONIC CLAIMS SUBMITTED, USING MY (OR THE ENTITY'S) MEDICAID PROVIDER
IDENTIFICATION NUMBER.
(Signature)
(Date)
(Typed Name and Title)
STATE OF NEW YORK
COUNTY OF
On this day of , 20
,before me personally came , to me known and known to me to be the
individual described in and who executed the foregoing instrument, and (s)he
acknowledged to me that (s)he executed the same.
(SEAL)
NOTARY
PUBLIC
Electronic Billing Certification Statement
Instructions
Field (1): ETIN (Magnetic Supplier Number)
Please indicate the ETIN under which the claims are being transmitted.
Field (2): BILLING SERVICE NAME
If applicable, enter the name of the billing service that the provider is enrolled with. If not using a billing service, leave this field blank.
Field (3): DATE
Enter the date the Certification Statement is signed and notarized (same date as Field 7).
Field (4): PROVIDER NAME
Enter the name of the provider whose signature is being notarized.
Field (5): PROVIDER NUMBER
Enter the 8-digit Medicaid provider ID number which was assigned by the Department of Health at the time of the provider's enrollment. This must be the individual provider number, not a group number or license number.
Field (6): SIGNATURE
Enter the signature of the individual indicated in Field 4. The signature must be original.
Field (7): DATE
Enter the date the Certification Statement is signed and notarized.
Field (8): NAME AND TITLE
Print the name and the title of the individual whose signature appears in Field 6.
Field (9): NOTARY PUBLIC
To be completed and signed by the Notary Public. Certification Statements that are not notarized cannot be accepted by the fiscal agent.
PLEASE NOTE:
Electronic Billing Certification must be renewed annually. Renewal documents will be provided prior to certification expiration.